Med info
When Does Vision Improve After Retinal Detachment Surgery?
Retinal Detachment Overview
The retina is the curved inner back layer of the eye, lined with light‑sensitive cells.
Retinal detachment means the retina has pulled away from the back wall of the eye.
Retinal detachment surgery aims to reattach the retina to the back of the eye and seal any tears or holes in it. The success rate is high: in about 9 out of 10 retinal detachment surgeries, the retina can be reattached.
Older adults are at higher risk of retinal detachment.
If a detached retina is left untreated, it can cause permanent vision loss.
See also: Electroretinography and Optic Nerve Tests
The Retina
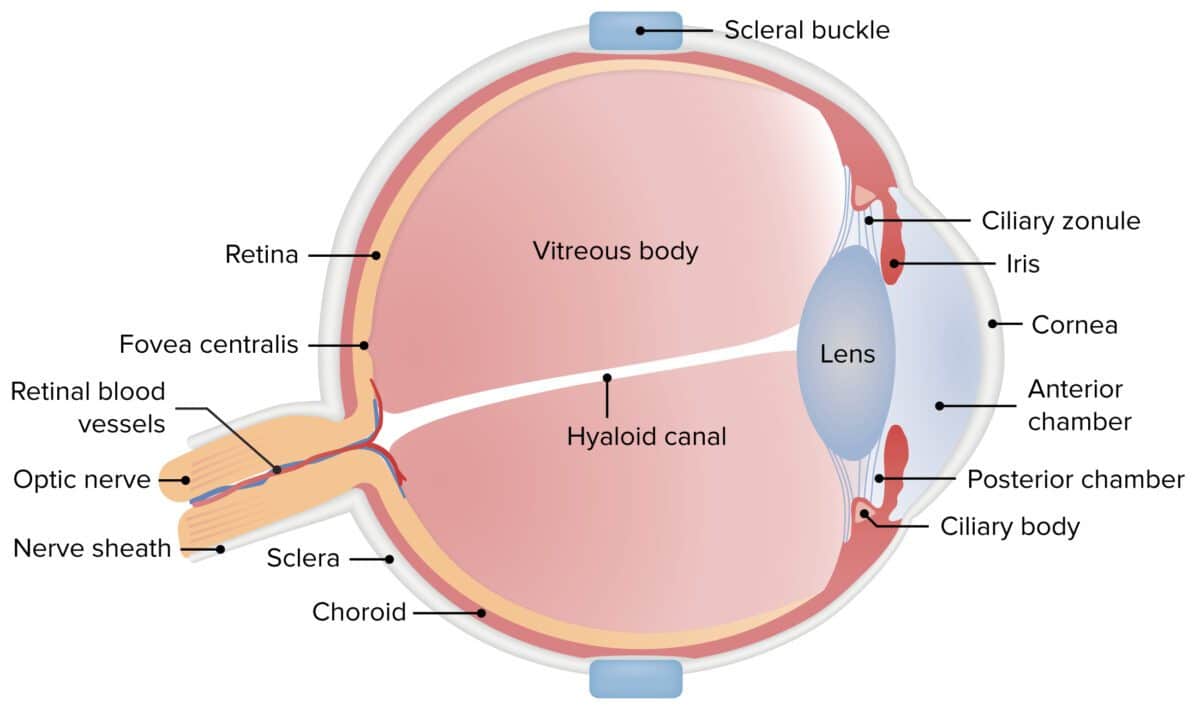
The retina is the innermost layer of the eye wall. It is made up of light‑sensitive cells called rods and cones, which detect shape, color, and patterns.
From the inside, the retina is supported by the vitreous gel that fills the eyeball behind the lens. On the outside, the retina is attached to the choroid, the middle vascular layer of the eye that is rich in blood vessels.
The nerve fibers leaving the retina bundle together to form the optic nerve, which carries visual information to the brain.
See also: The Retina | Everything You Need to Know About Retinal Detachment and Its Treatment
What Is Retinal Detachment?
Retinal detachment occurs when the retina separates from the underlying tissues (the choroid) that supply it with oxygen and nutrients. Once the retina is detached, it can no longer function normally, and vision starts to deteriorate or is lost in the affected area.
See also: Causes of Sudden High Eye Pressure
Causes of Retinal Detachment
The most common cause of retinal detachment is age‑related shrinkage of the vitreous gel. As the vitreous pulls away, it may tear the retina at a weak spot.
Once a tear or hole develops, fluid from inside the eye can pass through it and accumulate underneath the retina. This fluid lifts the retina off the choroid and leads to retinal detachment.
Eye trauma can also cause retinal detachment, although this is less common.
See also: Causes, Symptoms, and Treatment of Eye Swelling, Under‑Eye Puffiness, and Eyelid Swelling
Who Is at Risk for Retinal Detachment?
People at increased risk for retinal detachment include:
– (List of risk groups was not included in the original text, but typically includes: people with high myopia, previous eye surgery, eye trauma, family history of retinal detachment, etc.)
See also: Causes, Symptoms, and Treatment of Eye Swelling, Under‑Eye Puffiness, and Eyelid Swelling
Symptoms of Retinal Detachment
Retinal detachment itself is painless. However, a retinal tear may be accompanied by:
– Flashes of light in the affected eye
– A sudden shower or increase in dark floaters
– Blurred or distorted vision
When the retina detaches, it often causes a dark shadow, curtain, or veil in the peripheral vision, which can gradually spread and lead to complete loss of vision in that area.
You should see an ophthalmologist immediately if you experience any of these visual disturbances, because retinal detachment requires urgent surgery to prevent permanent vision damage.
Retinal Detachment Surgery
Retinal detachment surgery involves reattaching the retina to the back of the eye and sealing any tears or holes.
A retina specialist (vitreoretinal surgeon) will examine your eye and determine which surgical procedure is most appropriate for your specific condition.
Surgical Procedures for Retinal Detachment
There are several surgical techniques used to reattach the retina, including (depending on the case):
– Pneumatic retinopexy (injecting a gas bubble into the eye)
– Scleral buckle surgery
– Pars plana vitrectomy
See also: Retinal Detachment – Causes | Symptoms | Treatment
After Retinal Detachment Surgery
Immediately after surgery, you can expect:
– Blurred vision for a period of time
– Eye redness and mild discomfort
– Possible use of an eye patch or shield
– Eye drops to prevent infection and reduce inflammation
During the postoperative period:
– You may be asked to maintain a specific head position (for example, face‑down) if a gas or oil bubble was used to hold the retina in place.
– You must avoid strenuous activity, heavy lifting, and rubbing the eye.
– Follow‑up visits will be scheduled to monitor healing and retinal attachment.
Possible Complications of Retinal Detachment Surgery
The risks and potential complications depend on the type of procedure used, but may include:
– Cataract formation or progression
– Increased intraocular pressure (glaucoma)
– Recurrent retinal detachment
– Infection inside the eye (endophthalmitis)
– Bleeding
– Double vision or changes in refractive error
Long‑Term Outlook After Retinal Detachment
In most specialized centers, about 9 out of 10 retinal detachments can be successfully repaired with a single surgery. In the remaining cases, the retina may detach again and a second operation is needed. The final overall success rate is above 95%.
However, visual outcome does not depend only on whether the surgery technically succeeds. It also depends on how long the retina was detached, how extensive the detachment was, and which part of the retina was involved.
For example, if the macula—the central part of the retina responsible for sharp, central vision—was detached, full vision recovery is unlikely, even if the retina is successfully reattached.
See also: Is Eye Color Change Surgery Safe or Harmful, and Why?
Are There Any Other Treatments for Retinal Detachment?
Retinal detachment can only be treated with surgery. If it is left untreated, your vision is likely to worsen to a level where it cannot be restored.
You should see an ophthalmologist as soon as you notice any symptoms suggestive of retinal detachment.

See also: Frequently Asked Questions After My Experience With Retinal Detachment
Finally, if you are experiencing any vision problems or eye symptoms, book an appointment now and visit us to receive the best medical care at the most advanced and up‑to‑date eye clinics in Jeddah.


