Med info
The Importance of Accurate Diagnosis at Batal Eye Center in Yanbu
The Importance of Accurate Diagnosis in Ophthalmology
Accurate diagnosis in ophthalmology is the foundational and most critical step in developing an effective treatment plan for eye conditions. It enables the ophthalmologist to clearly identify the underlying cause of decreased visual acuity, blurred vision, or eye pain before initiating any form of therapy.
Through a comprehensive eye examination—which may include visual acuity testing, intraocular pressure measurement, and imaging of the retina and cornea—eye diseases can be detected at early stages, such as glaucoma, diabetic retinopathy, cataracts, and corneal disorders.
The earlier and more precise the diagnosis, the better the chances of selecting the most appropriate treatment modality, whether medical, laser-based, or surgical. This in turn enhances treatment success rates and reduces the risk of potential complications.
Accurate diagnosis also supports the development of a structured follow‑up plan and better control of systemic diseases that affect ocular health, such as diabetes and hypertension, thereby helping preserve vision and prevent irreversible vision loss.
For these reasons, consulting a qualified ophthalmologist and relying on advanced diagnostic technologies are key factors in achieving an accurate diagnosis and an effective treatment strategy for eye diseases.
Diagnostic Tests Your Eye Doctor Relies On
When designing a treatment plan, ophthalmologists depend on a series of precise diagnostic tests to accurately assess your eye condition and determine the most appropriate management options.
The assessment typically begins with a visual acuity test to measure how well you see and to evaluate the need for prescription eyeglasses or contact lenses. This is usually followed by intraocular pressure measurement to screen for glaucoma at an early stage.
Your doctor will then examine the back of the eye (fundus examination) using a specialized ophthalmoscope to carefully evaluate the retina, optic nerve, and retinal blood vessels.
In many cases, a refraction test is performed to assess refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. When a more detailed evaluation is needed, the ophthalmologist may order corneal or retinal imaging using Optical Coherence Tomography (OCT) to obtain high‑resolution cross‑sectional images.
Together, these comprehensive tests enable your eye doctor to develop an integrated treatment plan—whether based on medications, laser therapy, or surgery—aimed at providing the best possible long‑term protection for your vision.

Factors Influencing Treatment Selection
Choosing an appropriate eye treatment plan depends on several interrelated factors that must be carefully assessed before starting any medical or surgical intervention.
These include the nature of the ocular condition (such as myopia, hyperopia, astigmatism, cataract, glaucoma, or chronic dry eye), its severity and progression, and the extent to which it affects visual quality and the ability to carry out daily activities.
The patient’s age, overall health status, and the presence of chronic diseases—such as diabetes, hypertension, or autoimmune disorders—also play a decisive role in determining the most suitable type and dosage of treatment.
Family history of eye diseases is taken into account as well, along with the results of specialized tests, including intraocular pressure measurement, fundus examination, corneal thickness assessment, and visual acuity testing.
In addition, the patient’s lifestyle, occupational demands (such as prolonged screen use or frequent night driving), and their anticipated adherence to using eye drops or attending regular follow-up visits significantly influence the choice of the optimal treatment plan.
A clear understanding of these factors enables the ophthalmologist to design a personalized, safe, and effective treatment strategy that aims to achieve the best possible visual outcome while minimizing long‑term complications.
Comparing Available Treatment Options
Comparing eye treatment options starts with an accurate assessment of the patient’s condition. The choice of management plan can range from medicated eye drops to control dryness or mild inflammation, to laser procedures for correcting refractive errors such as myopia, hyperopia, and astigmatism, and may extend to microsurgical interventions in more advanced cases like cataracts or certain retinal diseases.
The ophthalmologist relies on a comprehensive eye examination—including visual acuity testing, corneal and retinal evaluation, and intraocular pressure measurement—to determine the safest and most appropriate treatment.
Important factors such as the patient’s age, lifestyle, presence of chronic conditions like diabetes or hypertension, and previous response to treatment are also taken into account.
The goal of this comparative approach is to select an integrated treatment plan that provides the best possible visual outcome with the lowest risk of complications, while emphasizing regular follow‑up to maintain long‑term ocular health.
The Patient’s Role in the Success of the Treatment Plan
The patient plays a central role in the success of any ophthalmic treatment plan, as adherence to medical instructions is the single most important factor in preserving vision and improving eye health.
This starts with carefully following the prescribed schedule for eye drops, and using prescription glasses or contact lenses exactly as directed by the ophthalmologist, without stopping medications or adjusting doses without prior medical advice.
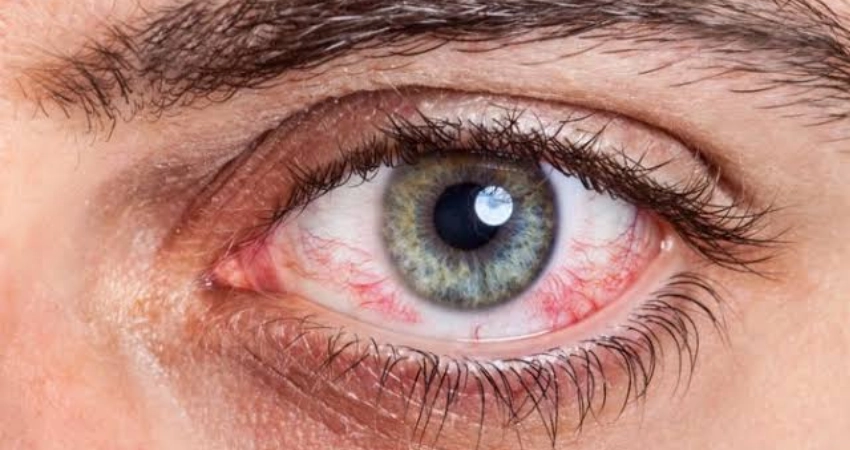
Informing the doctor promptly about any new symptoms—such as blurred vision, dry eyes, eye pain, or persistent redness—also allows for early adjustment of the treatment plan before the condition worsens.
Patients can further enhance the effectiveness of treatment by adopting a lifestyle that supports ocular health, including a diet rich in antioxidants, avoiding smoking, limiting screen time, and using blue-light filters and artificial tears when needed.
A patient who understands their condition, asks questions during ophthalmology visits, and keeps up with regular eye examinations is more likely to achieve the best possible outcomes from the treatment plan and to prevent long‑term complications of eye diseases.
Follow-up After Starting Treatment
Monitoring the eye condition after starting treatment is a cornerstone of any ophthalmic care plan. The ophthalmologist schedules regular follow-up appointments to assess how the eye is responding to medications, eye drops, or surgical procedures, to ensure visual stability, and to prevent disease progression.
During these follow-up visits, visual acuity is measured, intraocular pressure is checked, and both the cornea and retina are carefully examined. Based on these findings, the doctor may adjust drug dosages or introduce additional medications when needed to achieve the best possible outcome.
Regular follow-up is crucial for early detection of complications such as dry eye, ocular infections, or postoperative ocular hypertension. Early identification allows for timely intervention and reduces the risk of permanent optic nerve damage or irreversible vision loss.
Patients are strongly advised to adhere strictly to all scheduled follow-up visits and to contact their doctor immediately if they develop any unusual symptoms, such as sudden blurred vision, eye pain, marked redness, or the perception of flashes of light or floaters in their visual field.
Consistent follow-up with the ophthalmologist after starting treatment—combined with proper use of prescribed eye drops, contact lenses, or systemic medications—is the key factor in the success of the treatment plan and in preserving long-term eye health and vision.
At Batal Yanbu Medical Complex, every patient receives a customized treatment plan designed to achieve the best possible clinical outcomes.
At Batal Yanbu Eye Center, an individualized ocular treatment plan is developed after a comprehensive assessment of each case. This includes detailed visual acuity testing, intraocular pressure measurement, and advanced imaging of the retina and cornea using state-of-the-art diagnostic technologies.
The ophthalmologist relies on an accurate diagnosis to determine the most appropriate management options, whether prescription eyeglasses, contact lenses, topical medications, laser procedures, or surgical interventions such as refractive surgery, or cataract and glaucoma management.
Each treatment plan is tailored to the patient’s individual profile, taking into account age, lifestyle, and chronic conditions such as diabetes and hypertension, to ensure safe and effective care that preserves ocular health over the long term.
Patients are followed up regularly to monitor their response to treatment and to adjust the plan when needed, ensuring optimal therapeutic results, improved visual acuity, and enhanced quality of life, in line with the latest evidence-based guidelines and protocols in ophthalmology and eye surgery.



