Med info
Retinal Detachment: Causes, Symptoms, and Treatment
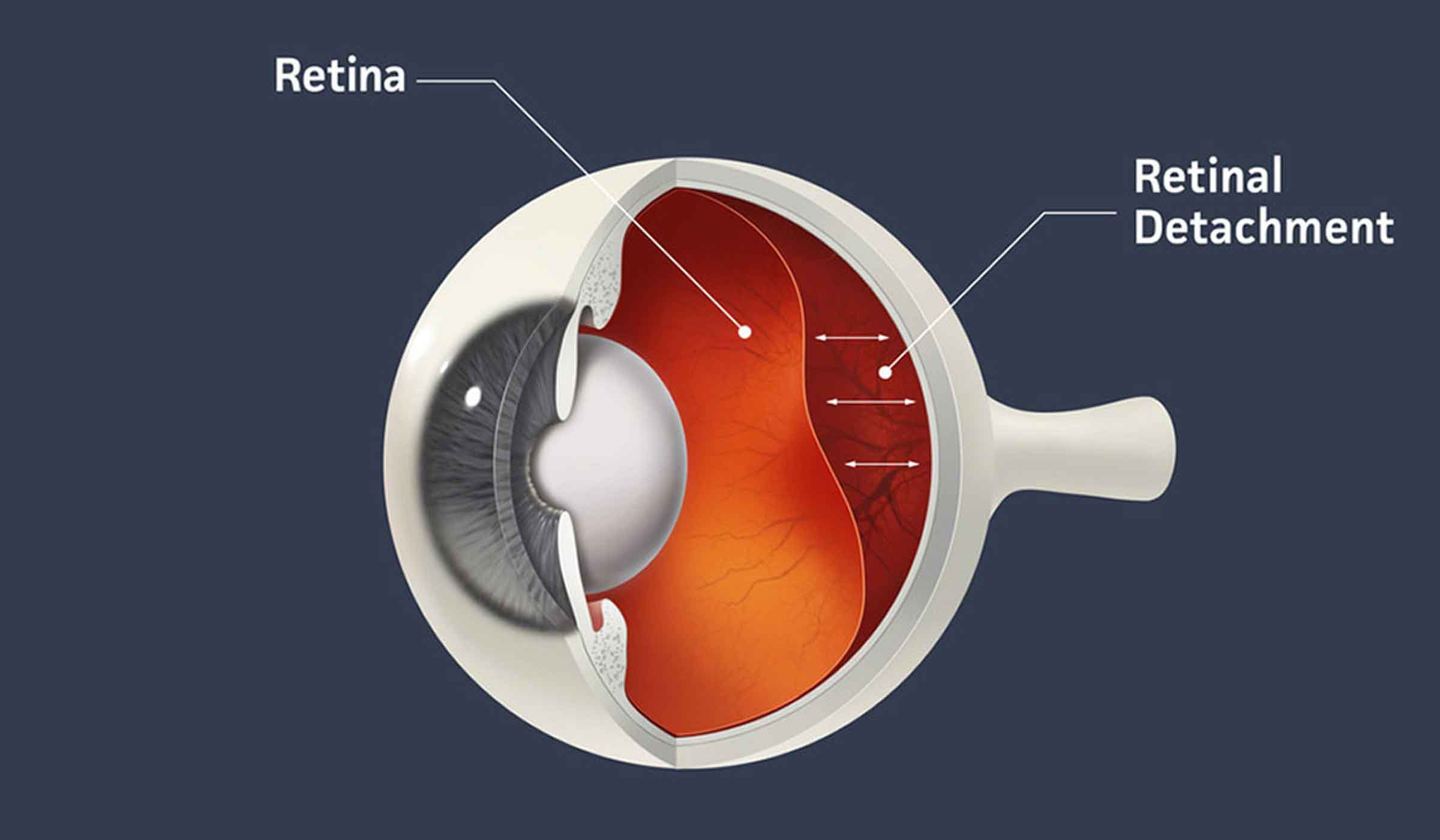
Retinal detachment is a serious eye condition that occurs when the retina pulls away from the back wall of the eye. The retina is a thin layer of light‑sensitive tissue lining the back of the eye that processes light signals. Doctors call this condition “retinal detachment” because once the retina separates, it can no longer function properly. If not treated promptly, it can lead to permanent vision loss. You should contact an ophthalmologist immediately if you suspect this problem.
Symptoms of Retinal Detachment
Retinal detachment is not painful, and it can happen suddenly without warning. You may notice:
<!– (The specific symptom list was not provided in the source text; typically it includes floaters, flashes, and a shadow/curtain over vision.) –>
Retinal Tear
The retina can develop a tear before it fully detaches. A torn retina usually causes the same kinds of symptoms seen with a complete detachment. When the retina tears, fluid inside the eye can seep through the tear and collect under the retina, lifting it away from the underlying tissue.
This is an emergency. See an ophthalmologist right away. In many cases, a retinal tear can be treated in the clinic with a laser procedure. If the retina has already started to detach, you may need more complex surgery to repair it.
Causes and Types of Retinal Detachment
There are three main types of retinal detachment:
Rhegmatogenous Retinal Detachment
This is the most common type. It occurs due to a break, tear, or hole in the retina. Age‑related changes often cause this: the vitreous gel that fills the eyeball shrinks and pulls away from the retina, creating traction that can lead to a tear.
Rhegmatogenous detachment can also result from eye trauma, previous eye surgery, or high myopia (severe nearsightedness).
Tractional Retinal Detachment
This type develops when scar tissue (fibrous tissue) forms on the surface of the retina and contracts, pulling on the retina and creating areas of elevation or tears. Diabetic retinopathy—damage to the blood vessels in the back of the eye caused by diabetes—is a common cause of tractional detachment.
Exudative Retinal Detachment
This is often related to inflammation or vascular problems. It happens when fluid accumulates under the retina without any tear or hole. The buildup of fluid pushes the retina away from the underlying tissue.
Common causes include leakage from abnormal or damaged blood vessels and swelling associated with conditions such as eye injury, intraocular inflammation, or age‑related macular degeneration (AMD).

Risk Factors for Retinal Detachment
Your risk of retinal detachment increases as you get older, and it is higher if you have any of the following:
(Specific risk factors were not listed in the source text; typically: high myopia, previous eye surgery, trauma, family history, etc.)
Diagnosis of Retinal Detachment
Your doctor will give you eye drops to dilate (widen) your pupils. Using a special lens and light, they will examine the inside of your eye to check whether the retina is torn or detached. They may also take imaging studies of the retina, such as fundus photography or an ocular ultrasound, especially if the view of the retina is not clear.
Treatment for Retinal Detachment
Your treatment may involve one or more of the following procedures:
(Procedures were not listed in the text; commonly: laser photocoagulation, cryotherapy, pneumatic retinopexy, scleral buckle, vitrectomy.)
About 80% to 90% of retinal detachment surgeries are successful, but some patients need more than one operation. It can take several months for your vision to recover as much as possible. Some people never regain full vision, especially in more severe or long‑standing detachments.
A detached retina will not heal on its own. Getting medical care as soon as possible gives you the best chance of preserving your sight.
See also: Retina | Everything You Need to Know About Retinal Detachment and How It Is Treated
Possible Complications of Retinal Detachment Surgery
Like any surgery, retinal detachment repair carries certain risks. Potential complications include:
(Not listed in the source; typically: infection, bleeding, cataract, elevated eye pressure, recurrent detachment, etc.)
Prevention of Retinal Detachment
See an ophthalmologist right away if you notice new floaters, flashes of light, wavy lines, dark spots, or any sudden changes in your vision. Regular comprehensive eye exams can also detect early retinal changes that you might not yet be aware of. Treating these problems early can prevent serious complications later.
If you have diabetes or high myopia (nearsightedness), have your eyes examined at least once a year. This helps protect the health of the retinal blood vessels and reduces your risk of vision‑threatening disease.
Use sports goggles with polycarbonate lenses if you play racquet sports or engage in activities that could cause eye injuries. You may also need protective eyewear if you work with machinery, chemicals, or tools—whether at work or at home.

Finally, patients often share with us their expectations and what they are currently experiencing. We work to address their concerns in ways that help them achieve the visual clarity they want and overcome vision problems that interfere with their daily lives. Do you have any eye problems that worry you? Book an appointment at our clinics now to receive the care that’s right for you.


