Med info
Preventing Glaucoma: What Everyone Needs to Know
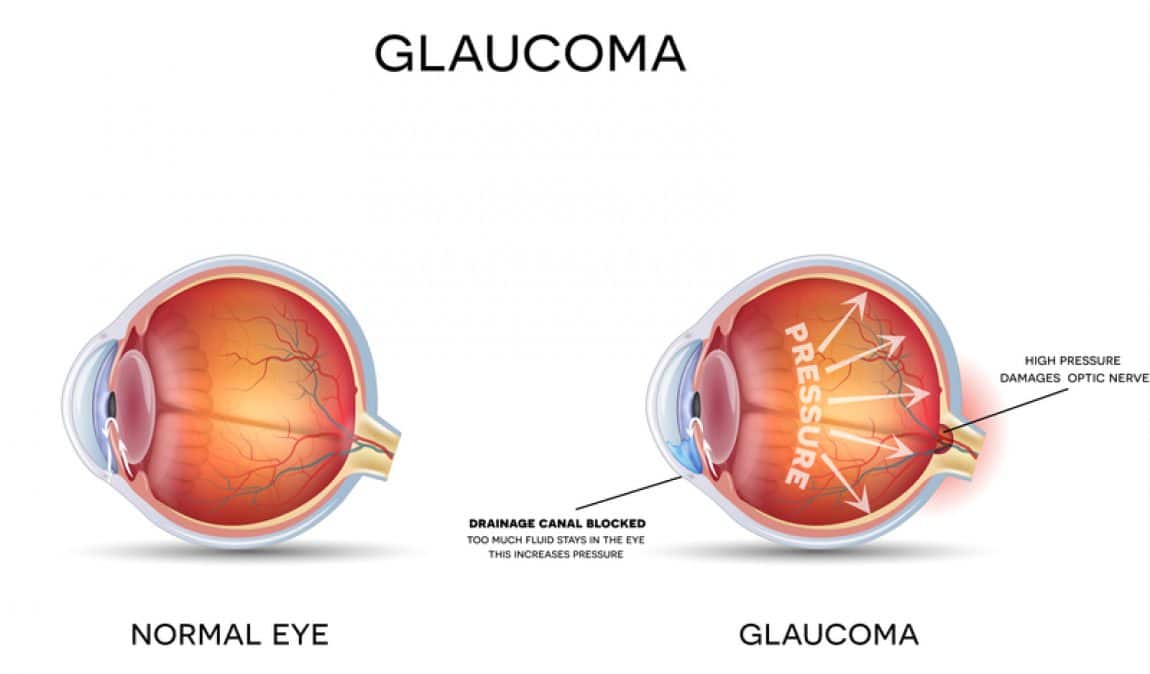
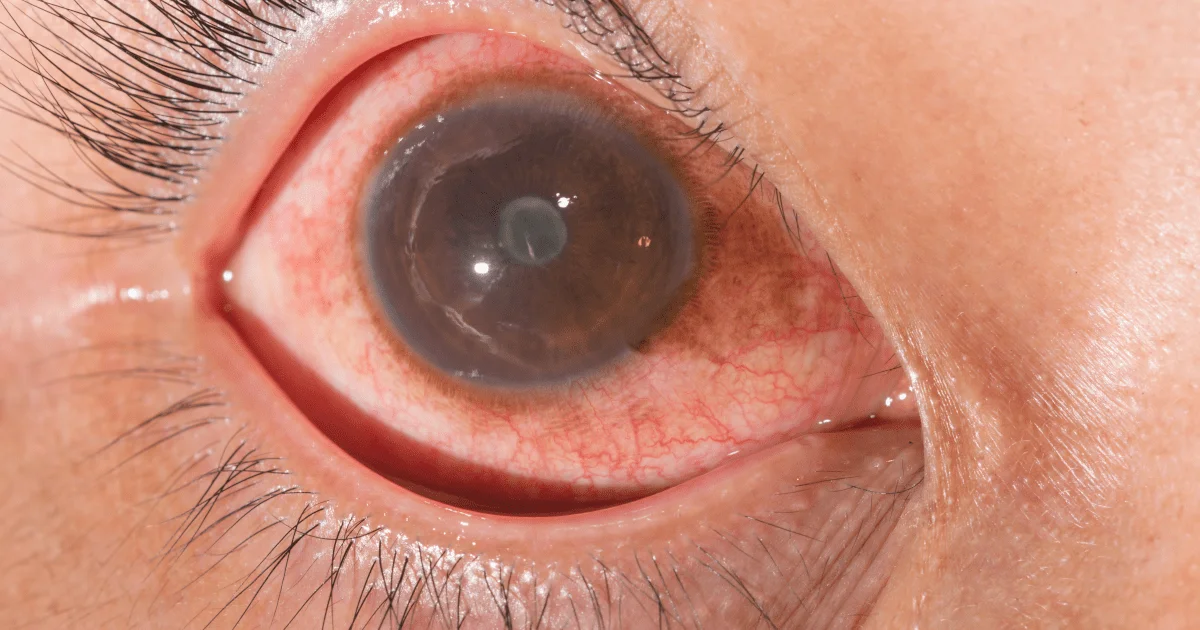
Glaucoma is a leading cause of blindness in people aged 60 and older. It occurs when fluid builds up inside the eye, increasing intraocular pressure (IOP) and causing irreversible damage to the optic nerve. This degenerative disease initially affects peripheral (side) vision, but if left untreated, it can eventually lead to complete loss of sight over time.
Most people with primary open‑angle glaucoma have no noticeable symptoms. When symptoms do appear, they usually show up late in the disease, which is why glaucoma is often called the “silent thief of sight.” The main warning sign is usually the gradual loss of side or peripheral vision.
Regular eye exams at the Eye Center in Batal Specialist Complex in Saudi Arabia—which is considered one of the best centers for early detection—are essential for catching the disease in its early stages and slowing its progression. Treatment is often delayed because early symptoms develop so slowly that they may not be noticed until the first acute attack occurs.
Read also: Differences Between a Child’s Eye Exam and a Standard Vision Test
What Are the Two Main Types of Glaucoma?
There are two main categories of glaucoma, and most cases fall into one of the following:
Primary glaucoma is not caused by another eye disease, while secondary glaucoma develops as a result of other eye conditions, trauma, or certain medications. Glaucoma usually affects both eyes, but the disease can progress more rapidly in one eye than in the other. In some cases, only one eye is affected—typically when glaucoma develops due to factors such as previous injury, inflammation, or steroid use in that single eye.
Read also: Femto LASIK Vision Correction Surgery

Different Types of Glaucoma
What Causes Glaucoma?
Elevated intraocular pressure is the main factor that leads to damage of the optic nerve in glaucoma. Normal‑tension glaucoma (where optic nerve damage occurs despite normal IOP) is discussed in the section on different types of glaucoma.
The optic nerve, located at the back of the eye, is the eye’s main nerve and carries the images we see to the brain. The eye itself is relatively rigid and round, like a basketball. Its shape and firmness are maintained by the pressure inside the eye (intraocular pressure), which normally ranges from about 8 to 22 mmHg.
When the pressure is too low, the eye becomes softer; when it is too high, the eye becomes firmer. The optic nerve is the part of the eye most vulnerable to elevated pressure because its delicate nerve fibers can be easily damaged—either by direct compression or by reduced blood flow to the nerve.
The front part of the eye is filled with a clear fluid called aqueous humor, which nourishes the structures in the anterior segment of the eye. This fluid is continuously produced by the ciliary body, which surrounds the eye’s lens.
From there, the aqueous humor flows through the pupil and drains out of the eye through tiny channels called the trabecular meshwork. These drainage channels lie in what is known as the eye’s drainage angle—where the clear cornea at the front of the eye meets the base (root or periphery) of the iris, the colored part of the eye.
The cornea covers the iris and the pupil in front of the lens. The pupil is the small black circular opening in the center of the iris. Light passes through the pupil, then through the lens, and on to the retina at the back of the eye. (See the diagram illustrating the eye’s drainage angle.)
The way aqueous humor is produced and drained from the eye is similar to a sink with the faucet running constantly: water is continuously added and drained. If the sink’s drain becomes blocked, the water level rises and may overflow. If that sink were a closed system—like the eye—where overflow is impossible, the pressure inside the sink would rise.
Similarly, if the eye’s trabecular meshwork becomes clogged or blocked, intraocular pressure can increase. Likewise, if the faucet is turned up too high, the sink fills faster than it drains. In a closed system, that again leads to elevated pressure.
If too much fluid is produced inside the eye, IOP can rise to damaging levels. In either situation, because the eye is a closed system, if excess fluid cannot be drained adequately, pressure builds up and may damage the optic nerve.
Read also: How to Care for Your Eyes After Laser Vision Correction
Risk Factors for Glaucoma
Glaucoma is often called “the thief of sight” because, as mentioned earlier, elevated eye pressure can slowly damage vision without causing obvious symptoms. For this reason, awareness and early detection are crucial. When diagnosed early, glaucoma can usually be managed successfully. While everyone is at some risk, certain groups have a much higher likelihood of developing glaucoma and should be examined more frequently by an ophthalmologist.
The ten major risk factors for glaucoma include:
How Do You Get Glaucoma?
Preventing Disease and Promoting Eye Health
Most glaucoma risk factors—such as age, ethnicity, and family history—are beyond a person’s control. That makes prevention and proactive eye care especially important, along with regular eye exams. Some key strategies to maintain healthy eyes include:
Read also: 5 Things You Should Know About the PanOptix Trifocal Lens
Read also: Retinal Tear – Causes, Symptoms, Treatment, and Complete Information
Please note that these tips do not guarantee prevention of eye disease and are not a substitute for regular comprehensive eye examinations. Nothing can replace a full ophthalmologic evaluation performed by a qualified specialist.
Read also: Early Signs of Cataracts and Everything You Need to Know
Can Cataracts Cause Glaucoma?
While cataracts themselves do not directly cause glaucoma, the two conditions can be linked in several ways:
How Successful Is Glaucoma Surgery?
The success rate of glaucoma surgery depends on several factors, including the type of procedure, the severity of the disease, and the patient’s individual response to surgery. Overall, however, glaucoma surgery can effectively lower intraocular pressure and slow or even halt disease progression.

My Experience With Glaucoma
Does Glaucoma Affect Both Eyes?
Glaucoma can affect one eye or both. However, having glaucoma in one eye significantly increases the risk of developing it in the other eye, because many glaucoma risk factors—such as elevated intraocular pressure—tend to be similar in both eyes. In some patients, glaucoma is more advanced in one eye, and the rate of progression may differ between the two eyes. This can result in differences in vision from one eye to the other.
Read also: Dacryocystitis – Causes, Symptoms, and Treatment
Treatment Options for Glaucoma
There is currently no cure for glaucoma, but its progression can usually be slowed using various treatments. The choice of therapy depends on how advanced the disease is and whether the patient is a suitable candidate for a particular treatment.
Treatment options fall into three main categories:
Glaucoma Medications
The most common treatment for glaucoma is prescription eye drops (oral medications may be used as a temporary measure before surgery). These medications aim to lower intraocular pressure either by improving the outflow of aqueous humor or by reducing its production.
For patients who struggle to use eye drops consistently, a dissolvable Durysta implant may be an excellent option. During a brief in‑office procedure, the ophthalmologist places the implant inside the eye, where it slowly and continuously releases medication to help lower IOP. Durysta’s targeted, sustained drug delivery—which can last for several months—eliminates the need for daily eye drops.
Laser Eye Surgery for Glaucoma
At Batal Specialist Eye Complex, we use a range of laser procedures to treat both open‑angle and angle‑closure glaucoma, tailoring the approach to each patient’s specific needs.
Laser procedures for glaucoma include endoscopic cyclophotocoagulation (ECP), selective laser trabeculoplasty (SLT), laser peripheral iridotomy (LPI), and transscleral or micropulse cyclophotocoagulation.
Minimally Invasive Glaucoma Surgery (MIGS)
In selected cases of mild to moderate glaucoma, patients benefit from minimally invasive surgical procedures, in which the surgeon makes a small incision and works on the internal drainage structures of the eye. Congenital glaucoma is primarily treated surgically because the underlying problem is a severely malformed drainage system that requires precise correction.
Read also: Keratitis – Risks, Symptoms, and Treatment

Glaucoma Prevention
Frequently Asked Questions
Is Glaucoma Hereditary?
The most common type of glaucoma, called primary open‑angle glaucoma (POAG), can have a genetic component. However, not everyone with a family history or genetic predisposition will develop the disease. Other factors—such as age, race, and overall health—also contribute to glaucoma risk.
What Does Vision Look Like With Glaucoma?
Glaucoma can cause gradual, permanent loss of vision, typically starting with peripheral (side) vision and later affecting central vision.
Can Glaucoma Cause Blindness?
Yes. Glaucoma can lead to blindness if it is not detected and treated early. It is the leading cause of irreversible blindness worldwide. It is estimated that up to 10% of people with glaucoma will still experience vision loss despite appropriate treatment. If left untreated or if treatment is delayed, glaucoma can result in total blindness.
Is Glaucoma Painful?
Generally, glaucoma itself is not painful. Because it often has no symptoms in its early stages, early diagnosis can be challenging. However, some forms of glaucoma—especially when eye pressure rises suddenly or markedly—can cause discomfort or even severe pain.
Is Glaucoma a Type of Cancer?
No. Glaucoma is not a form of cancer. It is a group of eye diseases that damage the optic nerve, which carries visual signals from the eye to the brain. This damage is usually related to increased intraocular pressure.
Read also: The Difference Between Wet and Dry Macular Degeneration

Whatever your visual symptoms, refractive errors, or eye problems may be, eye conditions are complex and require careful examination and appropriate treatment by a skilled, experienced ophthalmologist using effective medical technology to achieve the best possible outcome. Whatever eye disease you are facing, you can schedule an appointment at Batal Specialist Complex for a comprehensive eye examination and to begin addressing your eye problems, no matter how complex they may be. Please contact the Eye Center at Batal Specialist Complex in Saudi Arabia to book an appointment for eye care and to help reduce the risk of permanent vision loss.


