Med info
My Experience with Uveitis

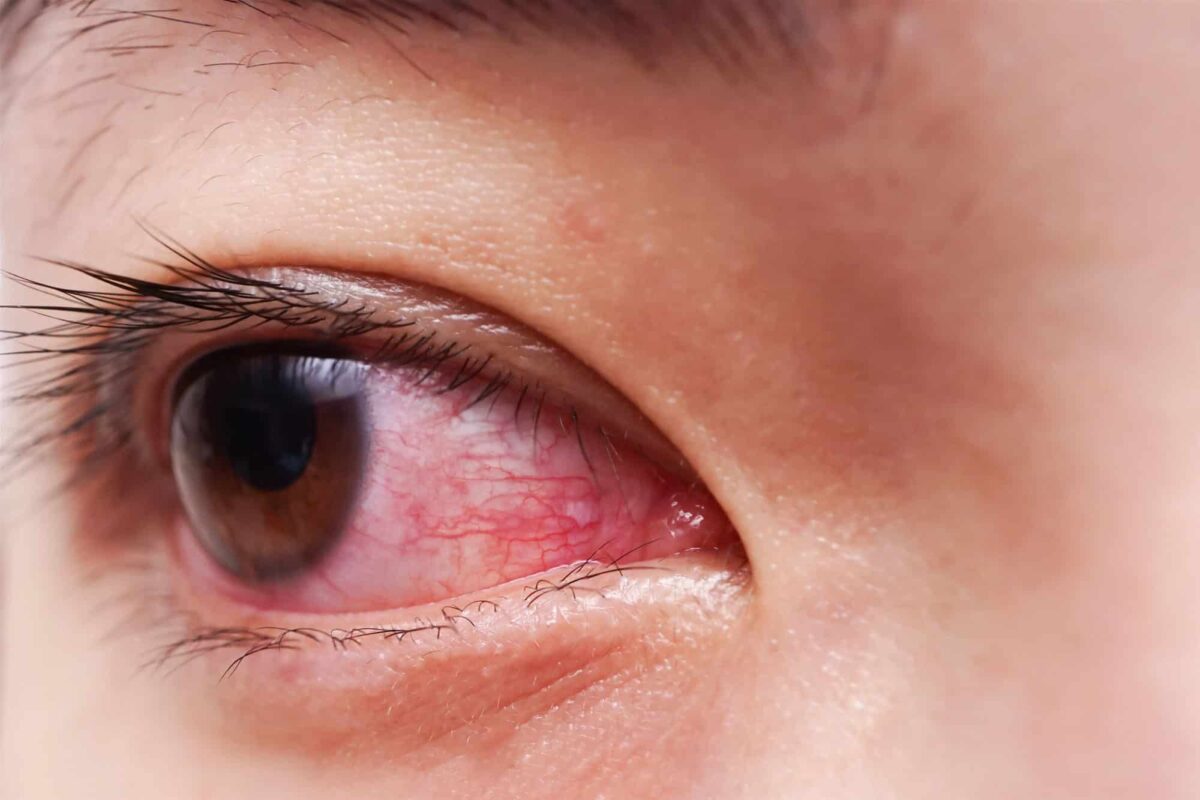
Uveitis is a common term for a group of inflammatory eye diseases that mainly affect the middle layer of the eye. The key symptoms are eye redness, eye pain, and some swelling. Uveitis can damage eye tissues and can affect people of all ages, but it is more common in women and tends to appear more with advancing age. That’s why it’s important to see an eye doctor as soon as you notice the first sign of a problem.
Read also: Symptoms of Optic Neuritis: Causes, Treatment, and Risks
What Is the Uvea?
The uvea is the middle, vascular layer of the eye, located between the white of the eye (sclera) and the retina. It includes:
– The iris: the colored part of the eye that controls how much light enters.
– The ciliary body: the structure that helps focus the lens and produces the fluid inside the eye.
– The choroid: the layer rich in blood vessels that nourishes the retina.
Causes of Uveitis
Uveitis may be caused by an eye injury (trauma) or by certain diseases such as HIV/AIDS, multiple sclerosis, rheumatoid arthritis or other forms of arthritis, syphilis, and tuberculosis. In many cases, however, the exact cause remains unknown.
If uveitis is not treated, it can lead to serious eye problems, including blindness. It can also cause complications such as cataracts, glaucoma, optic nerve damage, and retinal detachment. The following factors can increase the risk of developing uveitis:
– Autoimmune diseases (such as ankylosing spondylitis, sarcoidosis, inflammatory bowel disease)
– Certain infections (viral, bacterial, parasitic, or fungal)
– History of eye trauma or eye surgery
– Smoking
– Family or personal history of autoimmune or inflammatory conditions
Read also: Does Farsightedness Improve in Children? Everything About Hyperopia in Kids
Symptoms of Uveitis
Vision may become blurry, and there may be redness or pain in the eye. Symptoms may develop gradually, or you might wake up with them in the morning. The inflammation may affect one eye or both eyes, and it can involve any part of the eye, including the cornea (the clear front covering of the eye) and the white part known as the sclera. Possible symptoms include:
– Eye redness
– Eye pain or a deep aching sensation
– Blurred or decreased vision
– Sensitivity to light (photophobia)
– Excessive tearing or watery eyes
– Appearance of floaters (small spots or shadows moving in the field of vision)
– Headache, especially around or behind the eye
If you notice any of the symptoms above, you should consult an ophthalmologist immediately. The eye doctor will begin with a full eye examination and will ask about your medical history.
Types of Uveitis
Uveitis is usually classified according to the main area of inflammation:
– Anterior uveitis: affects the front part of the uvea, mainly the iris (iritis) or the iris and ciliary body (iridocyclitis).
– Intermediate uveitis: mainly affects the vitreous and the peripheral retina.
– Posterior uveitis: affects the back of the eye, including the retina and choroid.
– Panuveitis: inflammation involves all layers of the uvea (front, middle, and back of the eye).
Diagnosis
The ophthalmologist will ask about your symptoms, general medical history, and any existing health conditions. It is important to determine whether the uveitis is caused by an infection or related to an underlying systemic disease. If another condition appears to be triggering the uveitis, the eye doctor may refer you to a specialist (such as a rheumatologist or infectious disease specialist) to make sure you receive proper treatment.
The ophthalmologist will examine the eye using a special slit lamp (biomicroscope). When light is directed into the eye, the doctor can tell whether the area inside the eye is clear or hazy. If there is inflammation in the uvea, patients may feel some pain when the pupil constricts in response to the light.
When uveitis is present, white blood cells and protein can be seen in the eye’s fluid under the microscope, which confirms active inflammation. The doctor may also order blood tests, chest X‑rays, or other imaging (such as optical coherence tomography or fluorescein angiography) to look for underlying causes or complications.
Treatment of Uveitis
Most people with uveitis improve if they receive prompt and appropriate treatment. If it is left untreated, however, there is a higher risk of developing cataracts, glaucoma, band keratopathy, macular edema, and permanent vision loss.
Anti‑inflammatory medications are usually the first line of treatment. These are most often given as eye drops or eye ointments, and sometimes as oral medications or injections, especially when drops or ointments cannot reach the middle or back of the eye.
– Corticosteroids: These may be prescribed as eye drops (such as prednisolone acetate), oral tablets, or injections in or around the eye. Steroids are very effective in controlling inflammation, but before starting them, it is important to rule out corneal ulcers using a fluorescein staining test, because steroids can worsen certain infections.
– Anti‑infective medications: If an infection is causing the uveitis, antibiotics, antiviral, antifungal, or antiparasitic drugs may be used, depending on the organism involved.
– Immunosuppressive or immunomodulatory drugs: These may be recommended if symptoms are very severe, if there is a high risk of vision loss, or if the patient does not respond well to steroids or cannot tolerate them long term.
– Cycloplegic/mydriatic eye drops: Drops such as atropine or cyclopentolate are used to dilate the pupil and relax the ciliary muscle. They help the eye heal, reduce pain, and prevent the iris from sticking to the lens (posterior synechiae). During treatment, patients may experience blurred near vision and increased sensitivity to light (photophobia).
The main goal is to control the inflammation, protect eye structures, and preserve vision. After the acute inflammation is treated, the eye must be monitored regularly to prevent complications and permanent vision loss.
Uveitis itself is not contagious, but some of the underlying infections associated with it can be transmitted from person to person. You cannot “catch” uveitis from someone else, but you should be aware of and treat the conditions that might lead to it.
Complications
With rapid, appropriate treatment and close follow‑up, the risk of complications is greatly reduced. If complications do occur, they may include:
– Cataracts (clouding of the eye’s natural lens)
– Glaucoma (elevated eye pressure that can damage the optic nerve)
– Macular edema (swelling of the central retina responsible for detailed vision)
– Band keratopathy (calcium deposits in the cornea)
– Posterior synechiae (adhesions between the iris and the lens)
– Retinal detachment
– Optic nerve damage
– Permanent or severe vision loss

Read also: A Set of Questions After My Experience with Retinal Detachment


