Keratoconus Treatment with Laser Eye Surgery
Keratoconus is a progressive eye condition in which the normally round cornea gradually becomes thinner and bulges outward into a cone-like shape. This abnormal curvature prevents light from focusing properly on the retina, leading to blurred, distorted, and reduced vision.
Book your appointment or medical consultation today

Signs and Symptoms of Keratoconus
As the cornea becomes irregular in shape, it leads to progressive nearsightedness and irregular astigmatism, resulting in blurred, distorted, and unclear vision. Patients may also experience increased sensitivity to glare and bright light. In many cases, individuals with keratoconus notice frequent changes in their eyeglass prescription with each visit to the eye doctor. Keratoconus causes gradual thinning of the transparent cornea, leading to a cone-shaped bulging that weakens the eye’s ability to focus properly. This results in reduced visual clarity, severe light sensitivity, double vision, poor or absent night vision, and a rapid decline in visual acuity that often requires frequent changes in glasses or contact lens prescriptions within a short period of time.
Causes of Keratoconus
Keratoconus is a progressive eye condition in which the cornea becomes thinner and weakens near its center, causing it to bulge forward into a cone-like shape. As a result, light entering the eye is distorted, leading to blurred and irregular vision.
Although keratoconus does not cause complete blindness, it can lead to significant visual impairment if left untreated. With modern diagnostic methods and advanced treatment options, most patients with keratoconus are able to maintain good vision and live a normal, active lifestyle.
Keratoconus typically affects both eyes, although the severity and rate of progression often differ between them. It is not uncommon for one eye to be more advanced than the other. The cornea is the clear, dome-shaped surface at the front of the eye, responsible for bending and focusing light onto the retina.
Research suggests that keratoconus may be caused by a biochemical imbalance within the corneal tissue, particularly involving enzymes that protect the cornea from oxidative damage. This imbalance makes the cornea more vulnerable to damage from free radicals, leading to gradual weakening and forward bulging.
Several risk factors have been associated with the development of keratoconus, including genetic predisposition, which explains why the condition often appears in multiple members of the same family. Other contributing factors include excessive exposure to ultraviolet (UV) rays, chronic eye rubbing, poorly fitted contact lenses, and long-standing eye irritation or inflammation.
In the early stages of keratoconus, vision may be corrected with eyeglasses or soft contact lenses. However, as the condition progresses and the cornea becomes increasingly thin and irregular, standard glasses and soft lenses are no longer sufficient to provide clear vision, and more advanced treatment options become necessary.
Keratoconus and Laser Vision Correction (LASIK)
Keratoconus and LASIK are closely related topics, as LASIK and other laser refractive procedures such as PRK and SMILE are designed to correct nearsightedness and other refractive errors by reshaping the cornea. During this reshaping process, a portion of the corneal tissue is removed, which naturally makes the cornea thinner.
Keratoconus is a degenerative corneal condition that causes progressive thinning and irregular changes in the shape of the cornea. In certain individuals who are predisposed to this condition, removing too much corneal tissue during LASIK can increase the risk of a complication known as corneal ectasia, where the cornea becomes weakened and begins to bulge forward.
If you have keratoconus and are considering refractive surgery to correct nearsightedness or other vision problems, the first and most important step is a comprehensive corneal examination by an experienced ophthalmologist, preferably a specialist in corneal diseases.
In many cases, your doctor may recommend corneal cross-linking to strengthen and stabilize the cornea before considering any refractive procedure. Depending on the results of this treatment, it may then be possible to perform LASIK or another form of laser vision correction to reduce your dependence on glasses or contact lenses.
Specialized Contact Lenses for Keratoconus
As keratoconus progresses and the cornea becomes more cone-shaped, standard eyeglasses and soft contact lenses are no longer sufficient to provide clear vision. At this stage, specialized contact lenses are often required to achieve better visual correction and improve overall vision quality.
There are several advanced types of specialty contact lenses designed specifically for patients with moderate to advanced keratoconus. These lenses help create a smoother optical surface over the irregular cornea, allowing light to focus more accurately on the retina and significantly improving visual clarity.
Specialty contact lenses play an essential role in the non-surgical management of keratoconus and are considered one of the most effective vision correction options for patients who are not candidates for laser procedures or who require enhanced visual performance.
Treatment Options for Keratoconus
There are several effective treatment options available for managing keratoconus, depending on the stage and severity of the condition. These include eyeglasses, contact lenses, and surgical interventions such as corneal transplantation.
Eyeglasses
In the early stages of keratoconus, eyeglasses can often successfully correct nearsightedness and astigmatism. However, as the condition progresses and the cornea becomes increasingly irregular, glasses alone are no longer sufficient to provide clear and stable vision.
With precise examination and customized prescriptions, our specialists at Batal Specialized Center strive to optimize vision correction for patients in the early phases of keratoconus.
Contact Lenses
Contact lenses are commonly used to improve vision by creating a smoother optical surface over the irregular cornea. However, in approximately 5–10% of patients, keratoconus may progress to a stage where contact lenses are no longer effective or comfortable, making surgical options necessary.
While contact lenses do not slow the progression of keratoconus, they can significantly improve visual quality during stages when other methods are unable to provide adequate correction.
Surgical Treatment (Corneal Transplant)
Corneal transplantation is considered in advanced cases of keratoconus where other treatments no longer provide satisfactory vision. This procedure has a very high success rate, with approximately 98.1% of transplanted corneas remaining healthy in the first year and 97.5% still functioning well after four years.
A comprehensive eye examination with our ophthalmology specialists at Batal Center will help determine the most appropriate treatment plan tailored to your individual condition, with the goal of restoring vision quality and improving daily life.
Rigid Gas Permeable (RGP) Contact Lenses
Rigid gas permeable contact lenses are highly effective in correcting the abnormal optics caused by the irregular shape of the cornea in keratoconus. Unlike soft lenses, these lenses do not conform to the shape of the cornea, allowing them to create a smooth and regular optical surface that significantly improves visual clarity.
RGP lenses are considered an excellent vision correction solution for many patients with keratoconus. However, some individuals may find them uncomfortable to wear, especially during the initial adaptation period.
To enhance comfort and tolerance, RGP lenses can be worn over soft contact lenses (a technique known as piggybacking), or patients may benefit from hybrid lenses, which feature a rigid center for clear vision and soft outer edges for improved comfort.
Scleral Contact Lenses
In advanced cases of keratoconus where the cone becomes very pronounced, fitting traditional rigid contact lenses may become difficult. In such situations, patients can benefit from larger-diameter lenses that rest on the white part of the eye (the sclera) and vault over the cornea without touching its surface.
These lenses are known as scleral contact lenses. They are designed to create a smooth optical surface while avoiding direct contact with the sensitive cornea. In general, scleral lenses are very comfortable to wear and provide excellent visual clarity, making them an ideal option for patients with advanced or irregular keratoconus.
PROSE Lenses (Prosthetic Replacement of the Ocular Surface Ecosystem)
PROSE is a specialized subtype of rigid scleral lenses designed to replace or support the ocular surface ecosystem. This advanced prosthetic device is particularly beneficial in severe and complex cases of keratoconus where conventional contact lenses fail to provide adequate vision or comfort.
PROSE lenses are typically reserved as a last-line option before considering corneal transplantation. They create a protective, fluid-filled reservoir over the cornea, helping to improve vision, enhance comfort, and protect the ocular surface in advanced disease stages.
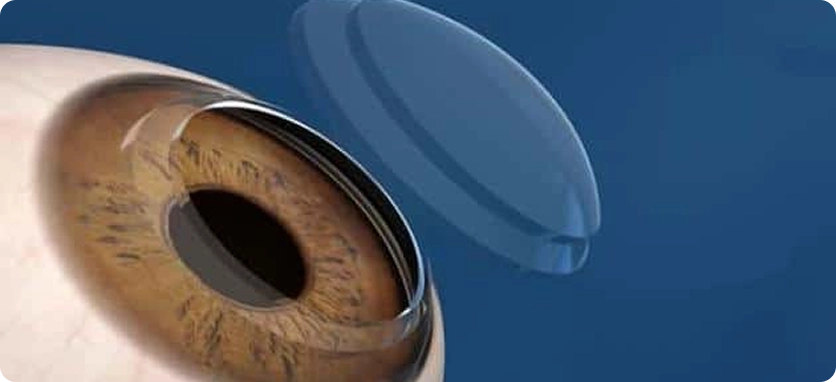
Corneal Collagen Cross-Linking (CXL)
Corneal cross-linking is an advanced treatment designed to effectively halt or slow the progression of keratoconus. The procedure works by strengthening the corneal tissue through a combination of riboflavin (vitamin B2) and controlled ultraviolet (UV) light, which together increase the rigidity and stability of the cornea.
During the procedure, the thin outer layer of the cornea (epithelium) is gently removed. The cornea is then saturated with riboflavin drops, followed by the application of UV light to activate the solution. This process creates new bonds between the collagen fibers within the cornea, reinforcing its structure and helping prevent further bulging. When performed early, corneal cross-linking can significantly slow or even stop the progression of keratoconus.
The treatment typically takes about one hour and is performed as an outpatient procedure. Patients may experience mild discomfort immediately after the treatment. A protective contact lens is placed on the eye for up to three days, and antibiotic eye drops are prescribed until the surface of the eye heals. This is followed by steroid eye drops for approximately 5 to 6 weeks to support proper recovery.
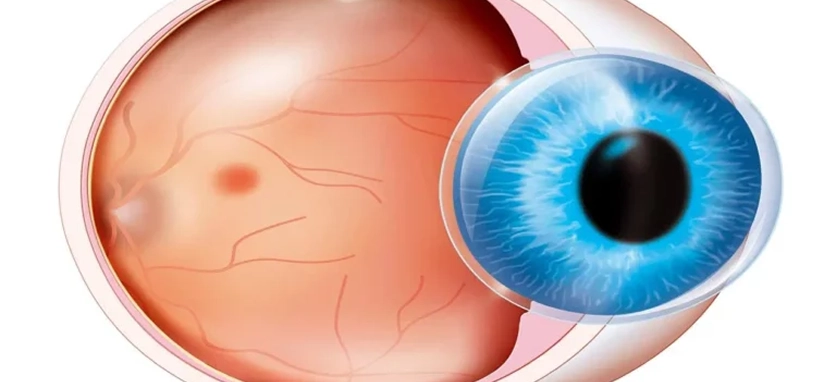
Corneal Transplant (Keratoplasty)
Corneal transplantation is considered only when all other treatment options have been exhausted. Approximately 10–20% of patients with keratoconus eventually require a corneal transplant. There are two main types of corneal transplantation: partial-thickness and full-thickness (penetrating) transplants. In most cases of keratoconus, full-thickness transplantation is the preferred option.
Corneal transplant surgery is a highly specialized procedure that typically requires admission for day surgery and is usually performed under local anesthesia, with the option of sedation for patient comfort. During the procedure, the surgeon carefully removes the damaged or irregular portion of the cornea and replaces it with healthy donor tissue, which is then secured in place with fine sutures.
Over time, your own corneal cells gradually grow and integrate into the donor tissue. The sutures are removed at a later stage as healing progresses. Full visual recovery after corneal transplant surgery for keratoconus can take up to one year, depending on individual healing response and postoperative care.
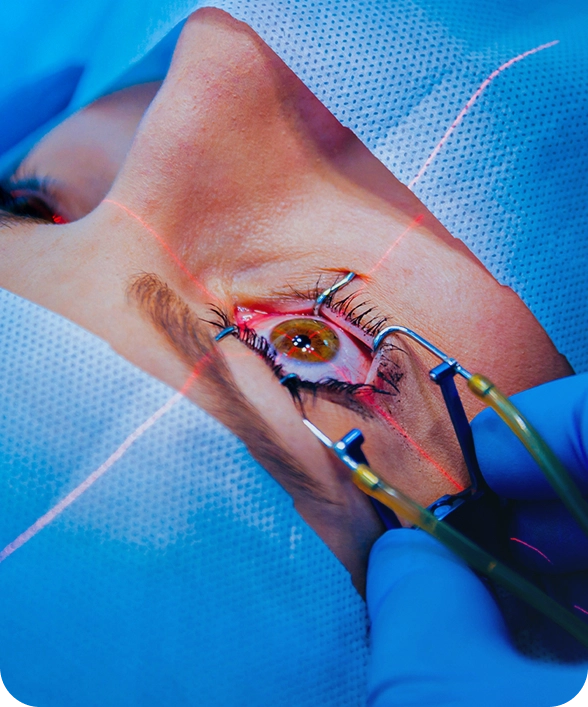
Keratoconus Surgery Procedure
The patient is able to return home on the same day of the procedure, which is performed as an outpatient treatment. The process typically follows these steps:
The ophthalmologist begins by numbing the eye with anesthetic eye drops, ensuring the patient feels no pain during the procedure. The thin outer layer of the cornea is then gently removed to allow the medication to penetrate deeper into the corneal tissue.
A special strengthening eye drop solution is applied to the cornea for approximately 30 minutes to prepare the tissue. After that, a controlled beam of ultraviolet (UV) light is directed onto the cornea for another 30 minutes to activate the treatment and reinforce the corneal structure.
At the end of the procedure, a therapeutic contact lens is placed over the eye to support healing and protect the surface. This lens is usually left in place for about one week while the cornea recovers.

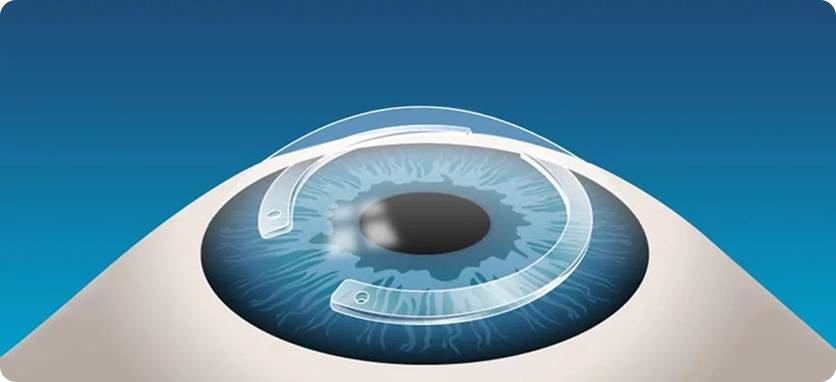
INTACS Corneal Ring Segments
INTACS are small, arc-shaped inserts that are surgically placed within the cornea to help flatten and reshape its curvature. By altering the shape of the cornea, these ring segments improve the way light enters the eye, leading to clearer and more stable vision.
The visual improvement achieved with INTACS remains effective as long as the rings stay properly positioned within the cornea. If the segments are removed or shift from their place, vision may return to its previous condition.
Clinical studies have shown that combining corneal cross-linking with INTACS implantation can produce excellent results in managing keratoconus, improving corneal stability, and enhancing visual quality in suitable patients.

Corneal Transplantation
Corneal transplantation is considered a less common treatment option and is usually reserved for advanced cases of keratoconus when other treatments are no longer effective. It is typically recommended when contact lenses fail to provide adequate vision due to severe thinning, scarring, or intolerance to contact lens wear.
During the procedure, the damaged cornea is surgically removed and replaced with healthy donor tissue. This replacement may involve the full thickness of the cornea or only the anterior (front) or posterior (back) layers, depending on the specific condition of the eye.
Visual recovery after corneal transplantation is gradual and may take more than a year to fully stabilize. In some cases, patients may still require specialized contact lenses after the transplant to achieve the best possible visual quality.
Keratoconus Diagnosis at Batal Specialized Eye Center
At Batal Specialized Eye Center, our ultimate goal is to provide our patients with the best possible vision, whether keratoconus is in its early stages or more advanced. Diagnosing keratoconus in its initial phases can be challenging, as many of its symptoms overlap with other eye conditions.
We are equipped with the latest diagnostic technologies, including advanced corneal topography and tomography systems, which allow us to detect early signs of keratoconus, accurately monitor disease progression, and distinguish it from other corneal disorders. Our experienced ophthalmologists carefully evaluate each case and discuss the most appropriate treatment options tailored to the patient’s condition.

The Best Keratoconus Surgeons at Batal Eye Specialty Center
Cataract Surgery, Laser Vision Correction & Corneal Surgery
Dr. Mohammad Hantira is one of the leading names in the field of ophthalmology and eye surgery. He serves as an Assistant Professor (Honorary) of Ophthalmology at Umm Al-Qura University and is highly regarded within both the medical and academic communities for his expertise and contributions.
87 Comments
The Best Keratoconus Surgeons at Batal Eye Specialty Center
Batal Eye Specialty Center
Get Comprehensive Medical Care


Installments available up to 100% via Tamara & Tabby



