Med info
How Does a Keratoconus Patient See? | What Is It Like Living With Keratoconus?

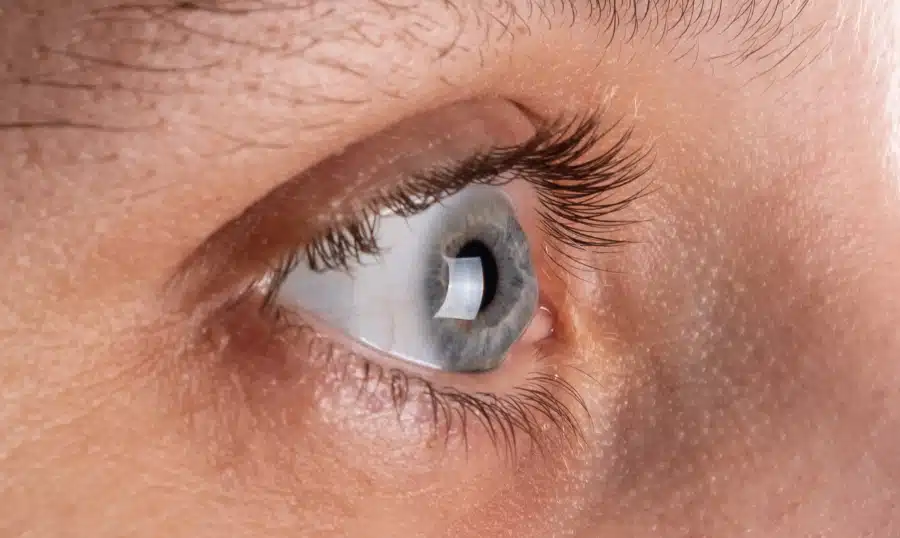
Before explaining how a person with keratoconus sees, it’s important to remember that keratoconus is a visual (eye) disorder characterized by progressive thinning and changes in the shape of the cornea.
The cornea is the thin, clear outer layer at the front of the eye. Under normal conditions it has a smooth, dome‑like shape. Gradual thinning of the cornea causes it to bulge forward in the thinnest areas, forming a cone‑shaped protrusion toward the center of the cornea.
People with this condition typically experience blurry or distorted vision, sensitivity to light (photophobia), and additional visual disturbances. Keratoconus usually begins around puberty and is often first noticed in teenagers or young adults.
The exact underlying cause is not fully understood. The condition is most likely due to a combination of factors, including genetic and environmental influences. One known contributing factor is chronic eye rubbing.
In some cases, keratoconus may occur as part of a broader systemic disorder. In the early stages, keratoconus is usually managed with eyeglasses or contact lenses, and only a minority of patients will eventually require surgery. But how exactly does a keratoconus patient see?
Also read: Symptoms of Keratitis | Causes, Diagnosis, and Treatment
Typical Treatment Options for Keratoconus
In the past, rigid gas‑permeable (RGP) contact lenses were thought to slow or stop the progression of keratoconus. Today we know this is not true. In fact, traditional RGP lenses can be uncomfortable and irritating for many people with keratoconus.
Scleral lenses have become a much better solution. Instead of resting directly on the cornea, these lenses vault over the entire corneal surface and rest on the sclera, the “white of the eye.”
By avoiding direct contact with the cornea, scleral lenses provide significantly better comfort while offering excellent stability and greatly improved vision. At Batal Specialty Complex, there are advanced, leading‑edge treatments for all types of eye diseases, especially keratoconus.
Also read: Cornea Problems | What Are the Most Common Corneal Conditions?
Keratoconus
Signs, Symptoms, and How a Keratoconus Patient Sees
Keratoconus usually affects both eyes (bilateral), although the rate of progression and severity can differ from one eye to the other (asymmetric progression). This means one eye may be noticeably worse than the other. Symptoms typically appear during the teenage years or early adulthood (late teens to early twenties).
Keratoconus may gradually worsen over 10 to 20 years before stabilizing. In older adults, the condition usually does not continue to progress. Because of its progressive nature, patients often need frequent changes in their eyeglass prescription.
The cornea’s primary function is to act as the eye’s most powerful focusing lens. It bends (refracts) incoming light toward the lower‑powered internal lens, which then focuses the light onto the retina, a thin, light‑sensitive layer of cells at the back of the eye.
The retina converts light into specific nerve signals that are transmitted to the brain, where they are processed into visual images. For the cornea to properly transmit and focus incoming light, it must remain clear (transparent) and maintain a regular shape.
The abnormal cone‑like shape that characterizes keratoconus alters the cornea’s ability to focus light accurately onto the retina, leading to refractive errors and optical distortions.
Early on, keratoconus may cause mild blurry vision, an abnormal increase in sensitivity to glare or bright lights, and difficulty seeing at night (night vision problems). Some patients experience double vision (diplopia) or describe partial, incomplete “ghost” images around what they are looking at.
In some cases, there may be a noticeable reduction in visual clarity (visual acuity). As the cornea continues to change, patients often develop increasing difficulty with distance vision (myopia/short‑sightedness) and a further decline in visual sharpness.
The overall visual changes vary greatly from one person to another. The severity can range from mild visual impairment to more pronounced vision loss that significantly reduces the ability to see clearly, even with glasses or standard contact lenses. Some patients develop irregular astigmatism, where the curvature of the eye’s surface becomes uneven and distorted.
Also read: Acanthamoeba Keratitis | Causes, Diagnosis, Treatment, and Full Guide 2023
What Causes Keratoconus?
This visual disorder is known to be associated with several factors, such as:
Also read: Causes of Poor Vision | 9 Factors That Can Damage Your Eyesight
Corneal Transplant Surgery
Corneal transplantation (corneal graft) is reserved for severe cases. The procedure involves replacing the central portion of the patient’s cornea with healthy donor corneal tissue from a deceased donor. For people with advanced keratoconus, this surgery can significantly improve quality of life.
It is important to note that keratoconus is often almost symptom‑free in its early stages. In general, regular comprehensive eye examinations are strongly recommended, especially for those with a family history of keratoconus or other corneal diseases.

Whatever corneal defects or problems are present, this is a delicate medical condition that requires thorough evaluation and appropriate treatment by a skilled, experienced ophthalmologist using effective, modern diagnostic and therapeutic tools to achieve the best possible outcomes. Whatever eye condition you are dealing with, you can book an appointment at Batal Specialty Complex for a full eye examination and to begin addressing your vision problems, whatever they may be.





