Electroretinography (ERG) Test
Electroretinography (ERG) is one of the most advanced and precise eye diagnostic tests. It is used to detect serious eye conditions such as night blindness, retinal detachment, optic nerve inflammation, and other eye diseases that may lead to vision loss and require urgent medical intervention. At Batal Eye Specialty Center, we use ERG testing to diagnose sudden abnormalities in the retina and optic nerve. The test converts electrical signals generated by the retina and optic nerve into detailed data that helps our specialists evaluate the extent of retinal damage and monitor changes in retinal or optic nerve function.

Electroretinography (ERG) Test
Electroretinography (ERG) is one of the most advanced and precise eye diagnostic tests. It is used to detect serious eye conditions such as night blindness, retinal detachment, optic nerve inflammation, and other eye diseases that may lead to vision loss and require urgent medical intervention. At Batal Eye Specialty Center, we use ERG testing to diagnose sudden abnormalities in the retina and optic nerve. The test converts electrical signals generated by the retina and optic nerve into detailed data that helps our specialists evaluate the extent of retinal damage and monitor changes in retinal or optic nerve function.

Can Night Blindness Lead to Blindness?
Disorders affecting the optic nerve or retina can lead to serious complications, including partial or complete vision loss. As mentioned earlier, these complications may include night blindness, retinal detachment, or optic neuritis. The danger of diseases affecting these critical structures of the eye is that they often show no noticeable symptoms in the early stages. However, once symptoms appear, the condition can progress rapidly and may require immediate medical intervention, as delayed treatment can result in permanent vision impairment or blindness. Symptoms of serious eye diseases are often similar, and the only way to accurately determine the underlying cause is through comprehensive and detailed diagnostic examinations. In the following sections, we will explore some of these conditions and their treatment options.
Night Blindness
Disorders affecting the optic nerve or retina can lead to serious complications, including partial or complete vision loss. As mentioned earlier, these complications may include night blindness, retinal detachment, or optic neuritis. The danger of diseases affecting these critical structures of the eye is that they often show no noticeable symptoms in the early stages. However, once symptoms appear, the condition can progress rapidly and may require immediate medical intervention, as delayed treatment can result in permanent vision impairment or blindness. Symptoms of serious eye diseases are often similar, and the only way to accurately determine the underlying cause is through comprehensive and detailed diagnostic examinations. In the following sections, we will explore some of these conditions and their treatment options.
Diagnosing Night Blindness
Our specialists will ask the patient several questions about their medical history and perform a series of examinations and tests to identify the symptoms and underlying cause. These may include contrast sensitivity testing and blood tests to measure blood sugar levels and vitamin A levels in the body.
Electroretinography (ERG) is also considered one of the key diagnostic tools for detecting night blindness and evaluating retinal function.
Preventing Night Blindness
Prevention is always better than treatment. At Batal Eye Specialty Center, we recommend regular comprehensive eye examinations and wearing certified protective sunglasses that block blue light and 99% of ultraviolet (UV) rays to help protect your vision and reduce the risk of night blindness.
Treatment of Night Blindness
The treatment of night blindness depends primarily on its underlying cause. In some cases, it may be related to myopia (nearsightedness), where treatment can be as simple as updating your prescription glasses or contact lenses. In other cases, surgical intervention may be required, such as when night blindness is caused by cataracts.
Treatment always depends on accurately diagnosing the condition that led to night blindness. If retinal damage is suspected, additional tests performed by a retinal specialist may be required before determining the appropriate treatment plan.
At Batal Eye Specialty Center, our ophthalmologists perform a comprehensive eye examination and request advanced imaging and specialized tests before considering refractive surgeries such as LASIK or PRK, which reshape the cornea to improve vision.
Since night blindness is usually a symptom of underlying eye conditions, rather than a disease itself, treatment focuses on identifying and addressing the root cause, which may include:
Glaucoma or Glaucoma Medications
Glaucoma itself may cause night vision problems. Treating the condition with eye drops, laser therapy, or surgery can improve vision. However, some glaucoma medications may also reduce night vision, so treatment adjustments may be necessary.
Myopia (Nearsightedness)
Myopia can change over time and may cause blurred vision in low-light conditions, which can mimic night blindness. Updating your glasses or contact lens prescription is usually the solution.
Cataracts
Age-related cataracts can cause cloudy vision and poor night vision. Cataract surgery, which replaces the cloudy natural lens with an artificial intraocular lens, can significantly improve both daytime and nighttime vision.
Refractive Eye Surgery
If night vision problems occur after LASIK or PRK, your ophthalmologist may recommend anti-reflective coatings or other solutions to reduce glare and improve visual quality.
Diabetes
Your doctor will evaluate whether diabetic retinopathy is contributing to night blindness and determine the appropriate treatment, which may include medication, laser therapy, or surgery.
Vitamin A Deficiency
In some cases, night blindness may result from vitamin A deficiency. Treatment may include dietary changes and vitamin supplements prescribed by a physician.
Genetic Factors
If night blindness is caused by genetic conditions such as retinitis pigmentosa, which currently has no definitive cure, our specialists can guide you on coping strategies and safety measures to reduce risks and maintain quality of life.
Retinal Detachment
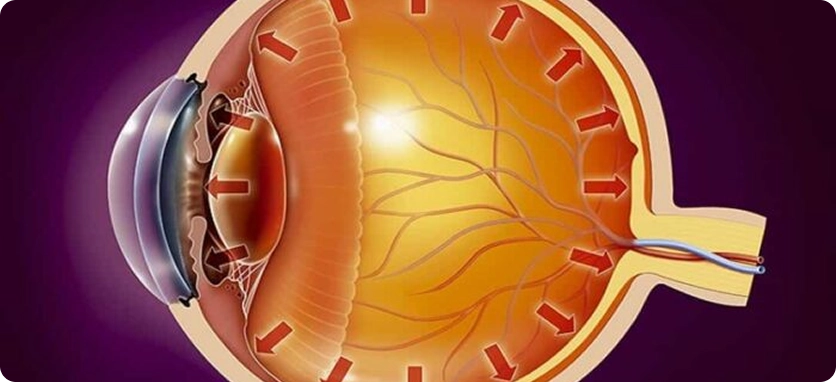
Retinal detachment occurs when the retina separates from its underlying support tissue at the back of the eye due to fluid accumulation behind the retina. This condition is often painless. Retinal detachment can have several causes, but the most common are aging and eye injuries. Eye trauma may result from severe injury or after eye surgery, such as cataract surgery.
People with myopia (nearsightedness) between the ages of 25 and 50 are also at a higher risk of developing retinal detachment.
Because retinal detachment is a serious condition that can lead to temporary or permanent vision loss, Batal Eye Specialty Center strongly recommends consulting an ophthalmologist immediately after any eye injury or if you experience symptoms of retinal detachment. Early diagnosis and treatment can help prevent vision loss.
We also recommend regular comprehensive eye examinations, especially for patients with high myopia. At Batal Eye Specialty Center, we offer electroretinography (ERG) and optic nerve testing, which play an important role in diagnosing retinal disorders.

Our Patients’ Experience with Retinal Detachment
Seeing a few small dark spots or wavy lines in your vision is usually normal and not a cause for concern. However, many patients diagnosed with retinal detachment at Batal Eye Specialty Center reported a sudden and significant increase in these spots and lines, along with a shadow or curtain-like blur blocking their vision.
If these symptoms appear suddenly, worsen, or are accompanied by persistent flashes of light or blurred vision, you should consult an ophthalmologist immediately. These may be early warning signs of retinal detachment and require urgent medical evaluation.

Examinations Required to Diagnose Retinal Detachment
During the initial examination, our specialists use medicated eye drops to dilate the pupil, allowing a detailed evaluation of the retina. In some cases, more advanced diagnostic tests may be required, such as ocular ultrasound or optical coherence tomography (OCT) using the latest available technology.

Laser Treatment for Retinal Detachment
After completing the necessary examinations and determining the severity of retinal detachment, the ophthalmologist will decide whether cryotherapy (freezing treatment) or laser treatment is the most appropriate option for your condition.
Our message to patients is reassuring: retinal detachment treatment is highly successful, with up to 9 out of 10 patients achieving positive outcomes when treated promptly.
Optic Neuritis
Optic neuritis can cause sudden vision loss, which may be partial or complete. It is often associated with eye pain that worsens with eye movement, changes in color vision, and blurred vision. This condition commonly affects young to middle-aged adults, and it is more frequent in women than in men.
Damage to the optic nerve may result from glaucoma or serious retinal diseases. Certain chemicals, medications, or nutritional deficiencies can also cause inflammation or damage to the optic nerve.
Vision can improve significantly when the underlying cause is identified and treated early with the appropriate therapy.
Optic Nerve Examination
Optic neuritis can significantly affect vision and may progress from simple inflammation to optic nerve atrophy and permanent tissue damage if left untreated, potentially leading to vision loss within days. In early stages, optic neuritis may not cause noticeable visual problems, and its symptoms can resemble other eye conditions, which is why precise diagnostic testing is essential.
At Batal Eye Specialty Center, optic neuritis is diagnosed through a comprehensive eye examination, fundus examination, and assessment of the eye’s response to light. In some cases, the ophthalmologist may request brain MRI imaging to confirm the diagnosis, determine the treatment plan, and assess whether anti-inflammatory treatment is required or if the condition may resolve on its own.
Making this decision requires high clinical expertise and specialized ophthalmic evaluation.

Optic Nerve and Intraocular Pressure
Poor drainage of the fluid inside the eye can lead to elevated intraocular pressure (IOP). If high eye pressure persists for a long time, it can damage retinal nerve fibers and eventually lead to permanent vision loss or blindness.
For this reason, glaucoma diagnosis relies heavily on measuring eye pressure, and treating glaucoma is a key step in preventing optic nerve damage.
Vision loss usually occurs in the advanced stages of glaucoma, but early and effective treatment can prevent further deterioration of vision. At Batal Eye Specialty Center, we strongly recommend early glaucoma screening and regular eye pressure measurements to detect the condition as early as possible.
Glaucoma Treatment Options
Medical treatment for glaucoma typically starts with prescription eye drops to lower intraocular pressure. If eye pressure remains high despite medication, laser treatment or surgical intervention may be recommended to protect the optic nerve and preserve vision.

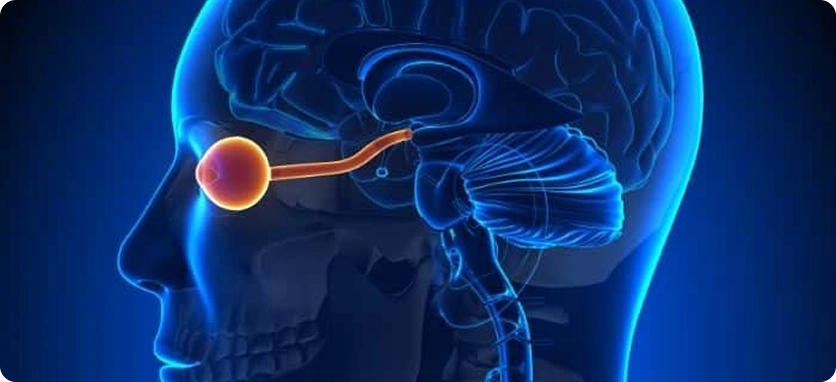
The Relationship Between the Optic Nerve and the Retina
The optic nerve is located at the center of the retina and is responsible for transmitting visual signals from the retina to the brain. Damage to the optic nerve can lead to several retinal disorders and vision problems.
Optic neuritis is particularly concerning because its symptoms often appear suddenly and can worsen within days. The good news is that appropriate treatment can lead to significant improvement within 4 to 6 weeks in most cases.
Our patients tell us that our attention to detail and personalized guidance make them highly satisfied with the medical care they receive. You can access our services by booking an appointment via our phone numbers, social media channels, or by subscribing to our patient service on WhatsApp.
Overview of Electrophysiology Tests in Ophthalmology
Vision is the result of electrical signals transmitted between the retina and the part of the brain responsible for vision. Electrophysiology tests are used to evaluate how effectively the optic nerve pathway transmits these visual signals.
These tests measure the electrical activity generated in the eye when viewing visual stimuli, helping specialists assess retinal and optic nerve function with high precision.
Electroretinography (ERG)
Full-field electroretinography measures the electrical response of the retina when viewing different patterns or flashes of light. It evaluates how well cone cells function, which are responsible for detecting light and color, and also assesses other retinal cells.
Full-field ERG can help detect conditions such as:
Retinal damage caused by medications or toxic substances
Night blindness (difficulty seeing in low-light conditions)
Eye problems related to vascular diseases
Multifocal ERG (mfERG)
Multifocal ERG measures electrical responses in the central area of the retina and is used to detect:
Macular diseases not identified by full-field ERG
Unexplained central vision loss not detected by standard ERG
Certain types of retinitis pigmentosa
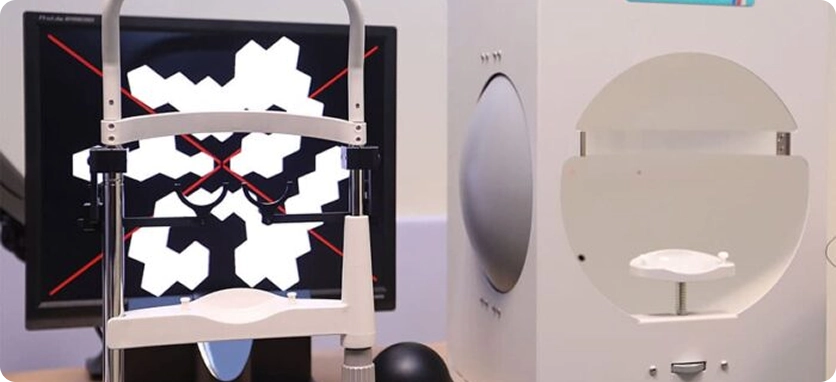
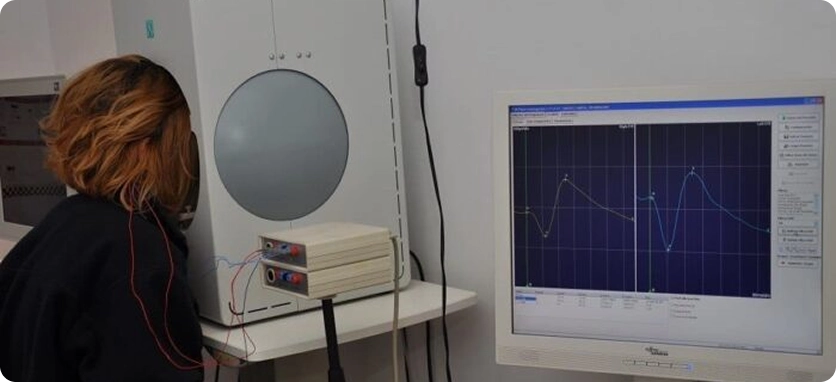
How Is the ERG Test Performed?
You may sit or lie down during the test.
Anesthetic eye drops are applied to numb the eye.
A small electrode is placed on the surface of the eye and on the face.
You will look at a screen showing flashes of light while the test records the electrical responses of the retina.
The electrical activity is displayed on a specialized device called an oscilloscope.
The test is performed in both light and dark conditions.
The entire examination takes about one hour.
Electrooculography (EOG)
Electrooculography (EOG) evaluates how well the electrical currents function across the entire eye. This test is used to assess certain eye and retinal conditions and helps detect disorders affecting retinal function.
EOG can assist in diagnosing conditions such as:
Inherited macular dystrophy
Retinitis pigmentosa
Visual Evoked Response (VER / VEP)
The Visual Evoked Potential (VEP) test evaluates the electrical activity along the entire visual pathway—from the eyes to the parts of the brain responsible for vision. It measures how the brain responds to visual stimuli and can help detect problems by analyzing brain wave responses while you look at specific visual patterns during the test.
How to Prepare for the VEP Test
No special preparation is usually required. However, please follow Batal Eye Specialty Center’s instructions before the test:
Follow your doctor’s dietary instructions to avoid low blood sugar.
Avoid caffeine for at least 12 hours before the test.
Wash your hair thoroughly before the test.
Do not wear jewelry or metal accessories near the head.

Risks of Eye Tests and Factors That May Affect Results
These tests usually cause little to no discomfort. In some cases, a person may not be able to undergo the tests, or the results may be less reliable if the instructions cannot be understood or followed. For example, certain vision tests may not be suitable for infants, young children, or individuals who cannot cooperate or follow instructions properly. Other factors may also prevent the test from being performed or may influence the results. Therefore, it is important to visit Batal Eye Specialty Center in Jeddah to discuss why the test is needed and what the results mean with your ophthalmologist.

Batal Eye Specialty Center Doctors
Oculoplastic & Aesthetic Eye Surgeon at Batal Eye Specialty Center
Over 25 years of experience in oculoplastic surgery and ophthalmic surgery.
87 Reviews
Batal Eye Specialty Center Doctors
Get comprehensive medical care


Installment plans available up to 100% via Tamara and Tabby



