Med info
Electroretinography (ERG): Purpose, Procedure, Results, and Importance at Batal Eye Specialty Center
What is Electroretinography (ERG)?
Electroretinography (ERG) is an advanced diagnostic test that measures the electrical activity of retinal cells in response to light. It allows the ophthalmologist to assess how well the different layers of the retina are functioning and to detect any abnormalities in their performance.
ERG is one of the key investigations for hereditary and degenerative retinal diseases such as retinitis pigmentosa, cone-rod dystrophy, and diabetic retinopathy. It is also used to investigate unexplained visual impairment in both children and adults.
The test is performed by placing a special electrode on the corneal surface or on the eyelid after numbing the eye with topical anesthetic drops. The eye is then exposed to controlled flashes of light, and highly sensitive equipment records the retina’s electrical responses and converts them into digital traces that can be analyzed.
ERG helps distinguish between optic nerve disorders and retinal diseases, determine the extent of photoreceptor damage, and guide treatment decisions and follow-up. For these reasons, electroretinography is considered an essential tool in modern ophthalmology and in the early diagnosis of retinal disorders.
Why is electroretinography an important test?
Electroretinography (ERG) is a key diagnostic test because it can accurately assess how well the retinal nerve cells are functioning, even before symptoms appear or any changes are visible on a standard fundus (retinal) examination.
This advanced test helps ophthalmologists diagnose inherited and degenerative retinal diseases at an early stage, such as retinitis pigmentosa, age‑related macular degeneration, and diabetic retinopathy.
ERG also plays a crucial role in investigating unexplained visual impairment, helping determine whether the problem originates in the retina itself, the optic nerve, or along the visual pathway in the brain.
In addition, it is used to monitor the progression of retinal diseases over time and to evaluate the effectiveness of different treatments, whether medical, surgical, or newer gene‑based therapies.
Because it is highly sensitive, painless, and safe, electroretinography has become an essential component of diagnostic and management protocols for retinal disorders in both children and adults, helping preserve vision as much as possible.

When does a doctor order an electroretinography (ERG) test?
A doctor may request an electroretinography (ERG) when there is suspicion of retinal cell dysfunction that cannot be identified through standard eye examination or fundus imaging alone.
This test is commonly used in cases of unexplained visual impairment, difficulty seeing at night (nyctalopia), or when hereditary retinal diseases are suspected, such as retinitis pigmentosa or cone-rod dystrophy.
ERG is also recommended in certain cases of strabismus in children, delayed visual development, and to assess retinal integrity before or after specific surgical procedures or medications that may affect photoreceptor function.
The test helps the physician evaluate how efficiently the retina is functioning, determine the extent of any damage, and choose an appropriate treatment plan or accurately monitor disease progression.
Electroretinography is considered an advanced and reliable diagnostic tool that contributes to the early detection of retinal disorders and improves the chances of preserving vision.
How is an Electroretinography (ERG) Test Performed?
Electroretinography (ERG) is usually performed in an ophthalmology clinic or a specialized retinal center. The test typically begins with dilating the pupils using medicated eye drops to allow the ophthalmologist a clear view of the retina.
Next, anesthetic eye drops are applied to the surface of the eye to minimize sensation and ensure the procedure is painless. The patient is then asked to sit or lie down in a comfortable position.
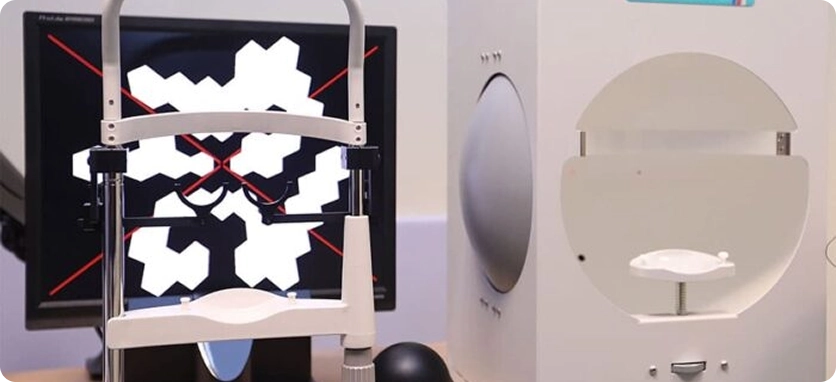
Small electrodes are placed either on the skin around the eye or directly on the cornea using a special contact lens. These electrodes are used to record the electrical responses generated by the retinal cells when they are stimulated by light.
The eyes are then exposed to flashes of light or specific visual patterns in a dark or dimly lit room, while the connected equipment accurately records the retina’s electrical activity.
An ERG test usually takes about 20–40 minutes. It is a safe and painless procedure that helps the ophthalmologist diagnose hereditary and degenerative retinal diseases, monitor disease progression, and plan the most appropriate treatment.
Is an ERG Test Painful or Dangerous?
An electroretinography (ERG) test is generally a safe and mostly painless procedure used to assess the health of the retina and the function of the cells responsible for vision.
The test works by recording the retina’s electrical responses to light. This is usually done after instilling a numbing eye drop, then gently placing a special contact lens or electrode on the surface of the eye or eyelid, which minimizes any discomfort.
Some patients may experience mild discomfort or a strange sensation in the eye during the test, but significant pain is not expected.
ERG does not cause permanent damage to the eye and does not negatively affect vision. Complications are extremely rare when the test is performed by an ophthalmologist in a reputable medical center.
Electroretinography is therefore considered a safe diagnostic tool that helps in the early detection of hereditary and degenerative retinal diseases, without exposing the patient to any meaningful risk.
What Do Electroretinography (ERG) Results Reveal?
Electroretinography (ERG) provides a detailed assessment of how efficiently the retinal nerve cells—particularly rods and cones—function and how they respond to light under different testing conditions.
By analyzing the shape of the electrical waveforms, their amplitudes, and the timing of their responses, physicians can identify inherited retinal dystrophies such as retinitis pigmentosa and cone–rod dystrophy, as well as conditions like diabetic retinopathy and retinal toxicity caused by certain medications.
ERG also helps differentiate between diseases of the optic nerve and disorders that primarily affect the retina. It is useful in evaluating the cause of otherwise unexplained visual loss, determining disease severity, tracking progression, and monitoring response to treatment.
When ERG responses are robust and within normal limits, this indicates healthy retinal function. In contrast, reduced or abnormal responses point to underlying dysfunction that requires careful evaluation and a tailored management plan.
Overall, ERG results serve as an advanced, objective tool that significantly improves the accuracy of diagnosing retinal diseases and enhances the chances of preserving vision over the long term.

The Difference Between Electroretinography and Other Retinal Tests
Electroretinography (ERG) differs from other retinal tests such as fundus photography, fluorescein angiography, and optical coherence tomography (OCT) in that it does not only show how the retina looks, but directly measures its electrical function.
During ERG, special electrodes are used to record the electrical responses of retinal cells to specific light stimuli. This makes it possible to detect hereditary and degenerative retinal disorders at an early stage, even when the fundus appears normal on conventional imaging.
In contrast, most other retinal and ocular tests focus mainly on assessing anatomical structures: retinal layer thickness, the presence of hemorrhage, exudation or tears, and other fine tissue details. These tests provide high‑resolution images, but they do not offer an objective measurement of retinal cell function.
For this reason, ERG is considered an important complementary investigation alongside other retinal examinations. It gives the ophthalmologist a clearer understanding of the integrity of the optic nerve, photoreceptors, and overall retinal function, supporting accurate diagnosis and helping to devise an appropriate treatment or follow‑up plan to preserve vision.
Why Batal Specialized Center is the Leading Facility for Electroretinography (ERG)
Batal Specialized Center is regarded as one of the top facilities for performing electroretinography thanks to its use of state-of-the-art, high‑precision equipment and advanced electrophysiological testing techniques. These include full‑field electroretinography (full‑field ERG), focal electroretinography (FERG), and visual evoked potentials (VEP), ensuring accurate diagnosis of retinal and optic nerve disorders.
The center brings together a select team of consultant ophthalmologists who specialize in retinal diseases and clinical electrophysiology of vision. They are highly trained in interpreting ERG and VEP results and correlating them with clinical findings to develop the most appropriate treatment plans.
Batal Specialized Center also adheres to strict infection control standards and follows patient‑friendly, safe procedures for all age groups, including children. Each step of the examination is clearly explained to help reduce anxiety and enhance the overall patient experience.
In addition, the center performs electroretinography in line with internationally recognized protocols, which reinforces the reliability of test results and supports accurate follow‑up of inherited and degenerative retinal diseases, diabetic retinopathy, and other complex visual disorders.
By combining deep clinical expertise, cutting‑edge technology, and professional patient care, Batal Specialized Center stands out as the ideal destination for anyone seeking precise and safe electroretinography‑based diagnosis.


