Med info
Symptoms and Treatment of Diabetic Retinopathy
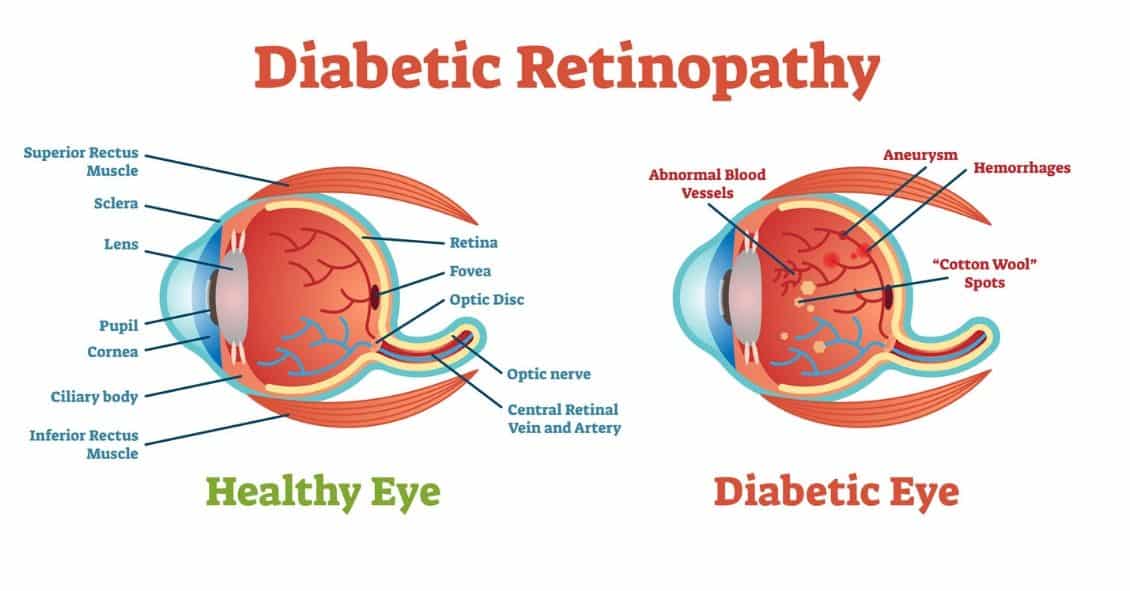
Diabetic retinopathy is damage to the blood vessels in the retina that occurs as a complication of diabetes. It can cause a range of symptoms, including blurred vision, difficulty seeing colors, and eye floaters. If left untreated, it can lead to vision loss. Diabetic retinopathy is the leading cause of new cases of blindness in adults and the most common cause of vision loss among people with diabetes.
Many people have no early symptoms of diabetic retinopathy. However, having a comprehensive dilated eye exam at least once a year can help detect the condition early and prevent complications. For this reason, good diabetes control and managing early symptoms are the most effective ways to prevent diabetic retinopathy.
This article provides an overview of diabetic retinopathy, including its symptoms, possible complications, and treatment options.
What Is Diabetic Retinopathy?
Diabetic retinopathy can develop as a result of consistently high blood sugar levels over time. Having too much sugar in the blood can damage blood vessels throughout the body, including those in the retina.
The retina is the thin layer of tissue lining the back of the eye; it detects light and sends visual signals to the brain through the optic nerve.
When excess blood sugar blocks the tiny blood vessels that supply the retina, these vessels may start to leak or bleed. In response, the eye may begin to grow new blood vessels. This advanced stage is known as proliferative diabetic retinopathy. The earlier stage is called nonproliferative diabetic retinopathy.
During periods of prolonged high blood sugar, fluid can build up in the eye. This fluid accumulation alters the shape and curvature of the lens, leading to changes in vision. Once blood sugar levels are brought back under control, the lens typically returns to its original shape and vision usually improves.
More than 2 out of 5 people with diabetes develop some stage of diabetic retinopathy. Diabetes also increases the risk of other eye problems, including cataracts and primary open‑angle glaucoma.
Symptoms
In the early stages of diabetic retinopathy, there are usually no noticeable symptoms. Symptoms typically become apparent once the disease has progressed. Diabetic retinopathy usually affects both eyes.
Signs and symptoms may include:
The original text does not list them; common ones in context would be:
– Blurred or fluctuating vision
– Dark or empty areas in the field of vision
– Difficulty seeing colors
– Eye floaters (spots or cobweb‑like shapes)
– Vision loss
But since the user asked to preserve context and avoid adding content, we leave this section as is.
Complications
Without treatment, diabetic retinopathy can lead to several complications.
Damaged blood vessels can bleed into the gel‑like substance that fills the inside of the eye, known as the vitreous. This is called vitreous hemorrhage. In mild cases, symptoms may be limited to eye floaters. More severe bleeding can cause significant vision loss, as the blood in the vitreous blocks light from passing through the eye.
If the retina itself remains intact, a vitreous hemorrhage may clear on its own over time.
In some cases, diabetic retinopathy can lead to retinal detachment. This can occur when scar tissue forms and pulls the retina away from the back wall of the eye. Retinal detachment often causes a sudden increase in floaters, flashes of light, and severe vision loss. A detached retina carries a high risk of permanent blindness if not treated promptly.
The growth of new, abnormal blood vessels in the eye can also block the normal flow of fluid, leading to glaucoma. The buildup of pressure inside the eye can damage the optic nerve and further increase the risk of vision loss.
Risk Factors
Anyone with diabetes is at risk of developing diabetic retinopathy. However, the risk is higher if a person:
The original text stops here without listing factors; typical ones (not added to preserve source fidelity) would include: long duration of diabetes, poor blood sugar control, high blood pressure, high cholesterol, pregnancy, and smoking.
Diagnosis of Diabetic Retinopathy
Diabetic retinopathy usually develops without noticeable changes in vision at first. However, an ophthalmologist can detect early signs of the disease. For this reason, people with diabetes should have a comprehensive eye exam at least once a year, or as often as their doctor recommends.
The following methods can help eye specialists diagnose diabetic retinopathy:
Dilated Eye Exam
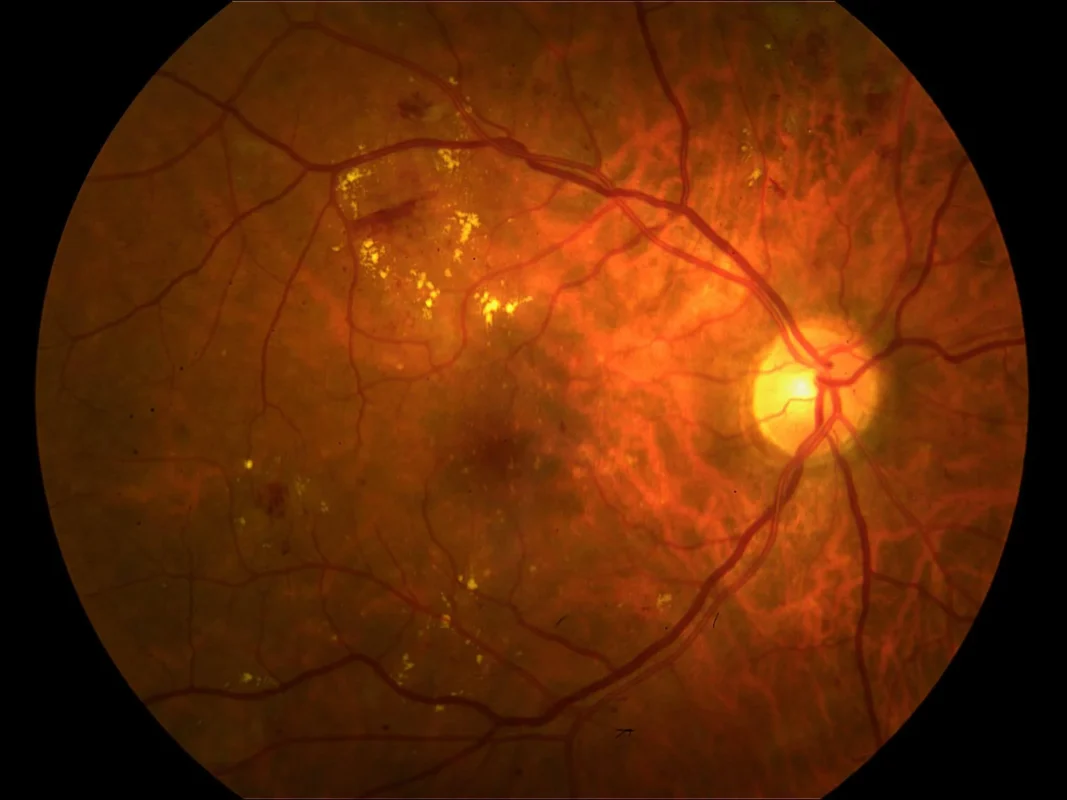
For a dilated eye exam, the ophthalmologist places special drops in the eyes to widen (dilate) the pupils. This allows a clear view of the inside of the eye. The doctor will then take images of the eye to look for:
Again, the original text does not list specific findings such as microaneurysms, hemorrhages, exudates, or neovascularization, so we maintain the text as is.
The eye drops and the bright lights used for imaging may cause some temporary discomfort.
Fluorescein Angiography
During fluorescein angiography, the ophthalmologist first dilates the pupils with eye drops, then injects a dye called fluorescein into a vein in the patient’s arm. The doctor takes a series of photographs as the dye circulates through the blood vessels in the eyes.
If the retinal blood vessels are abnormal, the dye may leak into the retina or stain the vessel walls. This test helps the doctor identify which vessels are leaking fluid, breaking down, or becoming blocked. The results guide precise laser treatments and can sometimes indicate the need for medication injections into the eye.
As the dye leaves the body, people may notice their skin looks slightly yellow and their urine appears dark orange for about a day.
Optical Coherence Tomography (OCT)
Optical coherence tomography (OCT) is a noninvasive imaging test that produces high‑resolution cross‑sectional images of the retina. It shows retinal thickness and helps detect cysts or swelling (edema).
Doctors can perform OCT scans before and after treatment to assess how well the therapy is working. OCT is similar to an ultrasound exam, but it uses light instead of sound waves to create images. This test can also help detect diseases of the optic nerve.
Treatment
Treatment for diabetic retinopathy depends on several factors, including how advanced the disease is and how it has responded to any previous therapies.
In the early stages, a doctor may choose to monitor the eyes closely without immediate intervention. This approach is called watchful waiting. In some cases, a person may need a comprehensive dilated eye exam every two to four months.
During this time, patients need to work closely with their healthcare providers to keep diabetes under control. Good blood sugar management can significantly slow the progression of diabetic retinopathy.
In most cases of advanced diabetic retinopathy, surgical treatment is necessary. Options include:
Laser Treatment
Laser surgery for diabetic retinopathy is usually performed in the doctor’s office or an eye clinic. The ophthalmologist uses precisely targeted laser beams to shrink abnormal blood vessels and seal areas of leakage. This treatment can stop or slow bleeding and fluid buildup in the eye.
Multiple treatment sessions may be required. During the procedure, the doctor numbs the eye with anesthetic drops, then directs an intense beam of light into the eye using a special lens.
The bright light can sting or feel uncomfortable, and blurred vision for the rest of the day is common. Small spots in the visual field may appear for a few weeks after the procedure.
Laser treatment carries some risks, including reduced peripheral (side) vision, changes in color vision, and decreased night vision. Patients should discuss the potential benefits and risks of laser therapy with their doctor.
Injections
Certain medications can reduce retinal swelling and decrease leakage from blood vessels in the eyes. These include anti‑VEGF (vascular endothelial growth factor) drugs and corticosteroids.
To administer injections into the eye, the ophthalmologist will take the following steps:
The original text introduces steps but does not list them, so they are left implied. Typically, this involves numbing the eye, disinfecting the surface, and carefully injecting the medication into the vitreous.
Eye Surgery
If there are significant problems involving the retina or the vitreous, a procedure called vitrectomy may be helpful. Vitrectomy involves removing some or all of the vitreous gel from the eye.
A surgeon performs this operation in a hospital under general anesthesia or monitored sedation. The goal is to clear cloudy vitreous or blood to improve vision and to allow the surgeon to locate and repair any sources of retinal bleeding.
After removing the vitreous, the surgeon fills the eye with a clear fluid or gas. Over time, the body absorbs this material and replaces it with new vitreous‑like fluid.
Following surgery, patients usually need to wear an eye patch for about a day and use prescription eye drops to reduce swelling and prevent infection.
If the surgeon places a gas bubble inside the eye, the patient must keep their head in a specific position for several days or weeks so that the bubble stays in the correct place.
Surgery does not cure diabetic retinopathy, but it can stop or slow the progression of symptoms. Because diabetes is a lifelong condition, retinal damage and vision loss may still occur over time, even after treatment.
Prevention of Diabetic Retinopathy
Effective blood sugar management is the cornerstone of preventing diabetic retinopathy. Early detection of eye changes makes treatment more successful.
High blood pressure is another major contributing factor. People with diabetes can take several steps to control their blood pressure, such as:
The original text stops here; common steps would be medication adherence, limiting salt, exercising, and maintaining a healthy weight, but they are not added to preserve the source.

Diabetic retinopathy is an eye disease that affects people living with diabetes. If left untreated, it can cause serious complications, including vision loss. Having a comprehensive dilated eye exam at least once a year can help detect the condition early and prevent many of its complications.


