Med info
Symptoms of Optic Neuritis: Causes, Treatment, and Risks
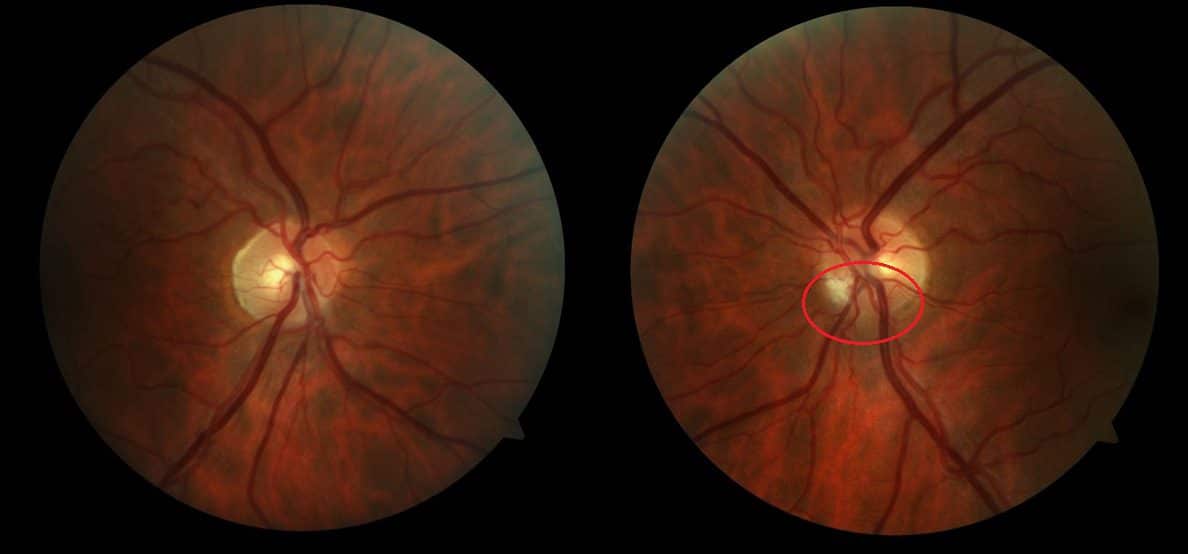
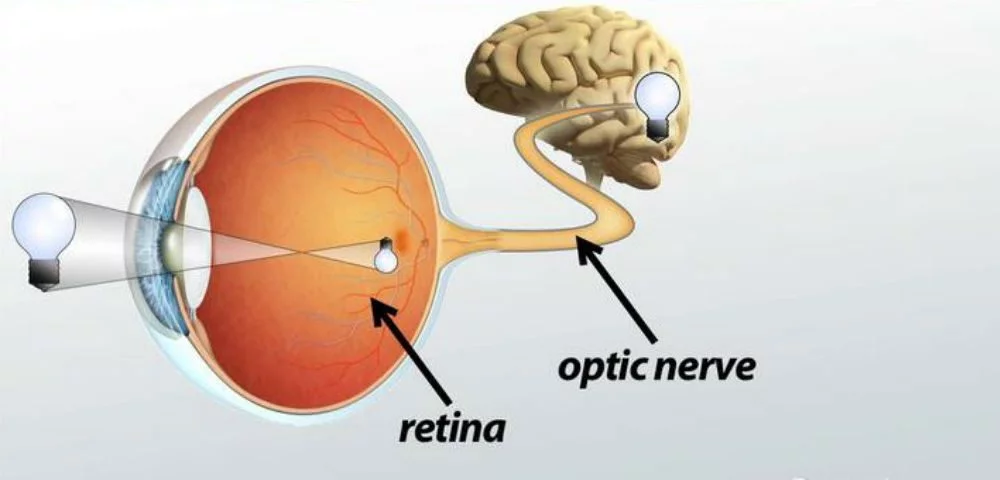
The optic nerve carries visual information from the eye to the brain. Optic neuritis (ON) occurs when this nerve becomes inflamed. It can appear suddenly as a result of an infection or a neurological disease. This inflammation usually causes temporary vision loss that typically affects only one eye. People with optic neuritis may sometimes experience pain, and although the condition can improve and the inflammation can resolve, vision often returns over time.
Other conditions can cause symptoms that resemble those of optic neuritis. To reach an accurate diagnosis, doctors often use tests such as Optical Coherence Tomography (OCT) and Magnetic Resonance Imaging (MRI). Optic neuritis does not always require treatment and can sometimes improve on its own. However, medications such as corticosteroids can help speed up recovery. Most people with optic neuritis regain full (or nearly full) vision within two to three months, although it may take up to 12 months for vision to recover as much as possible.
Read also: The Best Procedures and Techniques for Treating Retinal Detachment
Who Is at Risk for Optic Neuritis?
Your risk of developing optic neuritis increases if you:
Read also: Glaucoma Surgery
What Causes Optic Neuritis?
The exact cause of optic neuritis is not fully understood. Most cases are idiopathic, meaning no specific cause can be identified. The most common known cause, however, is multiple sclerosis (MS). In fact, optic neuritis is often the first manifestation of MS. It can also be triggered by infections or by an abnormal inflammatory response of the immune system.
Neurological diseases that can cause optic neuritis include:
Infections that may lead to optic neuritis include:
Other possible causes of optic neuritis include:
Read also: Causes of Eye Twitching and Personal Experiences with Eyelid Twitching
What Are the Symptoms of Optic Neuritis?
The three most common symptoms of optic neuritis are:
Other possible symptoms include:
Read also: Eye Pressure – Causes, Symptoms, Treatment Methods, and the Best Eye Drops
How Is Optic Neuritis Diagnosed?
Physical examination, symptoms, and medical history form the basis of diagnosing optic neuritis. To ensure appropriate management, your doctor may order additional tests to determine the underlying cause. Conditions that can lead to optic neuritis include:
There are also non‑inflammatory conditions that can mimic the symptoms of optic neuritis, such as:
Because of the close relationship between optic neuritis and multiple sclerosis, your doctor may recommend the following tests:
Read also: Everything You Need to Know About Eye Floaters – Causes and Treatment Options
How Is Optic Neuritis Treated?
Most cases of optic neuritis improve without specific treatment. If the inflammation is due to another medical condition, treating that underlying condition often leads to resolution of the optic neuritis.
Treatment options for optic neuritis include:
Using corticosteroids, such as intravenous methylprednisolone (IVMP), can have adverse effects. Rare side effects of IVMP include severe depression and pancreatitis. More common steroid-related side effects include:
Read also: The Retina – All You Need to Know About Retinal Detachment and How It Is Treated
What Is the Long‑Term Outlook?
Most people with optic neuritis have partial to near‑complete recovery of vision within 6 to 12 months. After that period, further improvement is less likely, and any remaining damage tends to be permanent. Even when vision appears to recover well, many patients are left with varying degrees of damage to the optic nerve.

Because the eyes are so critical to overall quality of life, any warning signs of possible permanent damage should be evaluated by a doctor before they become irreversible. These warning signs include worsening vision for more than two weeks and no noticeable improvement after eight weeks.
Read


