Med info
Treating Corneal Scratches: How to Treat a Scratched Eye

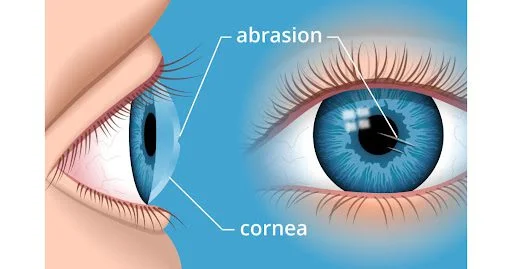
Treating a corneal scratch is very important. A corneal abrasion (also called a scratched cornea or scratched eye) is one of the most common eye injuries. The cornea is the clear front surface of the eye, and any scratch on it can damage the outer protective layer of corneal cells (called the corneal epithelium). This creates an open wound that increases the risk of a serious eye infection. For this reason, it’s crucial to see an ophthalmologist right away if you suspect a corneal scratch.
Because the cornea is the transparent front surface of the eye, a corneal abrasion can quickly disrupt its protective barrier. This open defect makes the eye more vulnerable to infection and possible vision‑threatening complications. Therefore, it is essential to seek immediate evaluation by an eye specialist, such as at the Eye Center in Al Batal Specialized Complex in Jeddah, if you suspect any scratch to the eye.
Read also: Treatment of Keratoconus | What Techniques Are Available?
What Causes a Corneal Scratch?
There are many possible causes of a corneal abrasion, whether large or small. Anything that comes into direct contact with the surface of the eye can potentially scratch the cornea. Common causes include tree branches, paper, makeup brushes, pets, fingers, workplace debris, sports equipment, and more. Sand, dust, and other tiny particles can also scratch the cornea—especially if you rub your eyes.
Dry eyes can increase the risk of corneal erosions, particularly if you routinely wake up with dry eyes. When the eyes dry out during sleep, the eyelids may stick to the corneal surface. When you wake up and open your eyes, the lids can pull off a small area of the corneal epithelium, causing a painful abrasion.
Contact lenses usually do not protect the eye from corneal scratches. In fact, if a contact lens is damaged or worn for too long, it can increase the risk of a corneal abrasion.
Any object that touches the eye’s surface can cause a corneal scratch—or even a retinal injury in more severe trauma—such as tree branches, paper, makeup brushes, pets, and fingers. Sand, dust, and other small particles can likewise injure the cornea.
Corneal scratches can also occur due to eye dryness, especially in people who frequently wake up with very dry eyes. If the eyes dry out during sleep, the lids can adhere to the cornea. Pulling them open may tear the epithelium. Regular contact lens wear does not prevent this, and worn‑out or damaged lenses further increase the risk. For proper management of corneal cracks and fingernail‑related eye scratches, it is better to visit the Eye Center at Al Batal Specialized Complex in Jeddah than to rely on home remedies.
Symptoms of a Corneal Abrasion
A corneal scratch often causes significant discomfort, watery eyes, redness, and marked light sensitivity (photophobia). The cornea is one of the most sensitive tissues in the body, so even a very small abrasion can feel extremely painful and much larger than it really is, as if there is a large, rough foreign body in the eye.
In addition to pain and a foreign‑body sensation, other signs and symptoms of a corneal abrasion include:
– Redness
– Excessive tearing
– Sensitivity to light
– Headache
– Blurry or reduced vision
– Eyelid twitching or spasms
– Occasionally, nausea
Any of these symptoms should prompt an evaluation by an ophthalmologist.
Retinal injuries (which are deeper, intraocular problems) can also cause severe visual symptoms, but in the context of a surface corneal scratch, the typical presentation is eye redness, pain, and light sensitivity, with the feeling that something is stuck in the eye.
Because these symptoms can overlap with other serious conditions, anyone experiencing signs of a corneal scratch should visit the Eye Center at Al Batal Specialized Complex in Jeddah, where experienced staff and advanced diagnostic equipment are available to manage recurrent corneal abrasions effectively.
See also: LASIK Surgery for Keratoconus
How Is a Corneal Crack Diagnosed?
It’s possible to scratch your own cornea without realizing exactly when it happened. For example, while trying to remove a contact lens, rubbing a finger directly over the cornea can create a small abrasion.
It is especially important to have an eye doctor examine the eye if there is any suspicion of a corneal or retinal injury, if symptoms are severe, or if they do not improve quickly. Professional assessment is needed to determine the extent of the abrasion and to rule out more serious eye damage.
What to Expect With a Scratched Cornea
People often instinctively rub their eyes when they feel something in them, but rubbing usually makes things worse. If you feel something in your eye, you can try rinsing it with a sterile solution rather than rubbing. Rubbing the eye can increase irritation, promote the spread of bacteria, and raise the risk of an eye infection.
The eye should be rinsed with sterile saline solution or a multipurpose contact lens solution, not tap water or bottled water. Microorganisms such as Acanthamoeba have been found in both tap and bottled water, and these pathogens can cause severe, vision‑threatening infections if they enter an eye that already has a corneal scratch.
After rinsing, if redness, pain, or the foreign‑body sensation persists, you should seek urgent care. A corneal abrasion can cause serious damage within hours if not managed properly.
To diagnose a corneal abrasion, an ophthalmologist will often place a numbing eye drop to make it easier to keep the eye open for examination. Another eye drop containing a temporary dye (such as fluorescein) may be used to highlight the defect. Under blue light and with a special examination microscope called a slit lamp, the scratch becomes clearly visible.
Depending on the cause of the abrasion and what the doctor observes during the exam, the eye’s surface may be gently swabbed to check for infection and guide appropriate treatment if needed.
See also: Corneal Transplant – Your Complete Guide
How Is a Corneal Scratch Treated?
Treatment of a corneal abrasion depends on the size and depth of the wound and its cause.
Mild, superficial abrasions can sometimes be treated with preservative‑free lubricating eye drops to keep the eye moist and comfortable while the cornea heals naturally. As a preventive measure, even small surface abrasions are often treated with antibiotic eye drops to reduce the risk of infection during healing. These superficial corneal scratches usually heal quickly, within about two to three days.
Some abrasions require an antibiotic ointment that stays on the eye longer than drops, along with a topical steroid to reduce inflammation and medications to relieve pain and light sensitivity. Larger and deeper abrasions take longer to heal and may leave a permanent corneal scar that can affect vision.
In some cases, scratched corneas are treated with a bandage contact lens. When used together with prescription eye drops, this special type of lens can relieve pain and, in some patients, speed up the healing process.
Standard contact lenses should generally not be worn over a corneal abrasion, because they can trap bacteria and greatly increase the risk of infection under the lens. Depending on the treatment plan and severity of the injury, the ophthalmologist may schedule a follow‑up visit as soon as 24 hours after the initial treatment.
When treated promptly, most corneal abrasions heal quickly without permanent vision loss. However, deeper scratches in the central cornea (directly in front of the pupil) can leave a scar and reduce visual acuity.
If left untreated, some deep abrasions can progress to a corneal ulcer, which may cause severe and sometimes irreversible vision loss. Injuries caused by organic material (such as plant matter or fingernails) particularly increase the risk of corneal ulceration.
It is very important to follow the eye doctor’s treatment instructions carefully and attend all recommended follow‑up visits. Not all corneal scratches heal perfectly; some may lead to recurrent corneal erosion and other complications that can affect vision, comfort, and overall eye health.
There are also ointments specifically used for scratched eyes that stay on the surface longer, as well as steroid drops to control inflammation. Healing time for a large, deep corneal abrasion is considerably longer. Bandage contact lenses, combined with prescription “scratch eye” drops, can provide pain relief and sometimes promote faster recovery.
Ordinary contact lenses should not be worn until the abrasion has fully healed, due to the increased risk of infection beneath the lens. Based on the treatment plan and the severity of the injury, the ophthalmologist will determine the appropriate schedule for follow‑up—often within 24 hours of the initial visit. With prompt, proper management, most corneal abrasions heal without long‑term vision problems, but deep central scratches can leave scars that reduce visual sharpness.
If recurrent corneal abrasions are not treated properly, they can progress to corneal ulcers. Injuries from organic material further increase this risk. Therefore, it is essential to follow the recommendations of the Eye Center at Al Batal Specialized Complex in Jeddah and attend all scheduled follow‑up appointments. Inadequate healing can lead to repeated corneal erosions and other complications that may compromise vision, comfort, and eye health.
Read also: When Does Vision Improve After Retinal Detachment Surgery?
How to Prevent a Scratched Eye
Many corneal abrasions can be prevented with simple precautions and common‑sense measures. For example, always wear safety glasses or protective goggles in work environments where airborne debris is present, especially in welding or grinding areas.
Similarly, protective eyewear should be used during yard work, when using power tools, and when playing sports, even if you wear contact lenses.
If you wear contact lenses, follow your eye doctor’s instructions closely about how long to wear them, when to replace them, and which cleaning and disinfecting solutions to use.

If you have corneal abrasions that seem to be related to dry eyes, consult an ophthalmologist and follow the recommended dry eye treatment protocol.
Read also: Signs of Successful Retinal Detachment Surgery


