Med info
Types of Eye Hemorrhage: Causes, Symptoms, and Treatment Options
What are the types of eye hemorrhage?
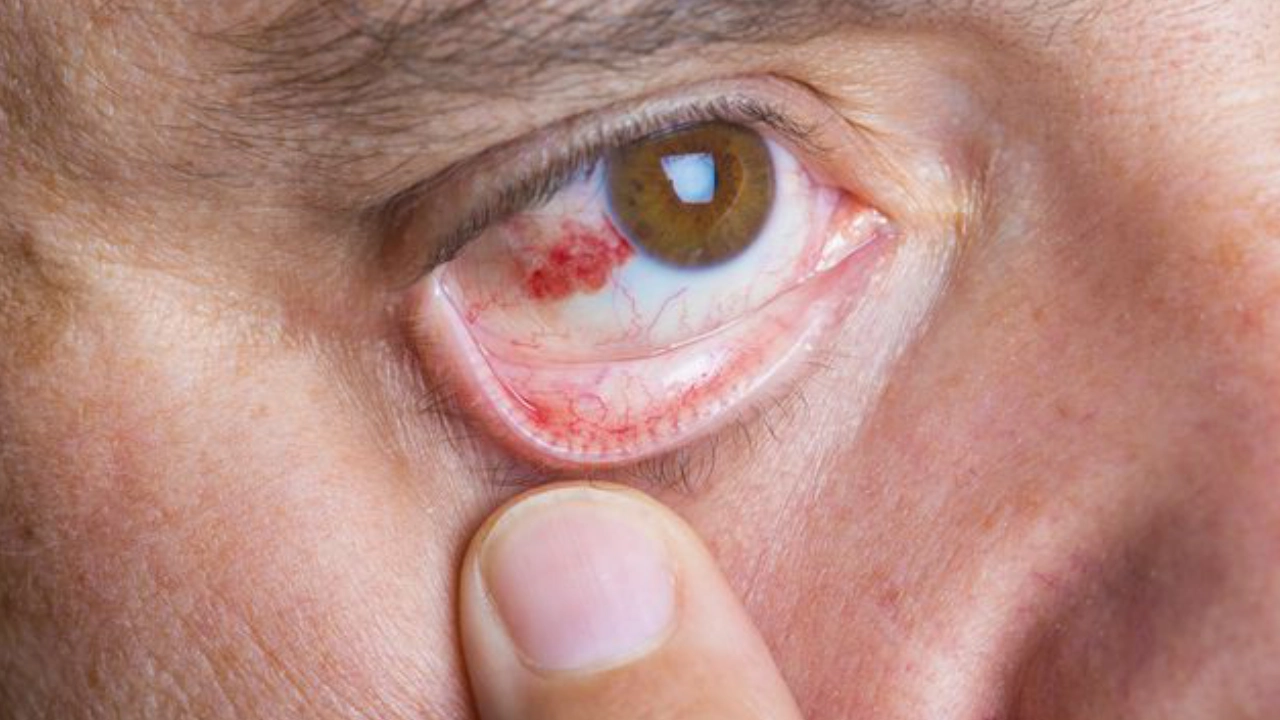
Eye bleeding can appear in several forms. The most common is **subconjunctival hemorrhage**, where a bright red patch develops on the white of the eye due to the rupture of tiny blood vessels, usually without pain.
Another type is **vitreous hemorrhage**, which occurs in the clear gel (vitreous humor) filling the center of the eye, and typically causes black floaters or severe haziness that clouds the vision.
There is also **retinal hemorrhage**, which affects the light‑sensitive layer at the back of the eye (the retina). It is often associated with conditions such as diabetes and high blood pressure and can lead to a gradual decline in visual acuity.
In addition, bleeding can occur in the anterior chamber of the eye, known as **hyphema**, where blood accumulates between the cornea and the iris as a result of injury or direct trauma. This is considered an emergency, as it may increase intraocular pressure and threaten vision.
Recognizing the different types of eye hemorrhage is crucial for identifying the cause early, seeking timely medical advice, protecting eyesight, and reducing the risk of complications.

Subconjunctival Hemorrhage
Subconjunctival hemorrhage is one of the most common and least serious types of eye bleeding. It typically appears as a bright red patch on the white part of the eye (sclera) and is not usually associated with pain or visual disturbance.
This condition occurs when tiny blood vessels rupture beneath the conjunctiva—the clear membrane covering the white of the eye. It is often triggered by severe coughing, sneezing, lifting heavy objects, high blood pressure, or vigorous eye rubbing.
In most cases, a subconjunctival hemorrhage is a minor condition that is not a cause for concern. It usually resolves on its own within one to two weeks without the need for specific treatment. Artificial tears may be used to relieve any associated discomfort or dryness.
However, if eye bleeding recurs, is accompanied by bleeding from other parts of the body, or is associated with visual problems, it is advisable to consult an ophthalmologist to rule out bleeding disorders or other underlying conditions.
Recognizing this type of eye hemorrhage and distinguishing it from more serious forms—such as vitreous hemorrhage or retinal hemorrhage—helps reassure the patient and ensures they receive appropriate guidance and timely management.

What is a subconjunctival hemorrhage?
A subconjunctival hemorrhage is a small collection of blood that forms beneath the transparent membrane covering the white of the eye (the conjunctiva). It is one of the most common and least serious types of eye bleeding.
It occurs when a tiny conjunctival blood vessel ruptures, leading to a sharply defined red or dark patch on the surface of the eye, similar in appearance to a bruise on the skin.
Although its appearance can be alarming, a subconjunctival hemorrhage usually does not affect vision, and it typically causes no pain or light sensitivity. In many cases, it is noticed incidentally when looking in the mirror.
It is classified as a superficial ocular hemorrhage and is distinct from deeper types of eye bleeding such as vitreous hemorrhage or retinal hemorrhage, as it does not usually involve significant damage to the internal structures of the eye.
Understanding the nature of a subconjunctival hemorrhage helps patients distinguish between minor conditions and those that require prompt ophthalmologic assessment within the broader context of ocular hemorrhages.
Causes of subconjunctival hemorrhage
The causes of subconjunctival hemorrhage range from trivial triggers to underlying medical conditions. All of them share a common mechanism: either a sudden rise in pressure within small blood vessels or structural fragility of these vessels.
Common triggers include severe coughing, forceful sneezing, vomiting, or heavy lifting, all of which can cause a sudden increase in venous pressure and lead to rupture of the fine conjunctival capillaries.
Subconjunctival hemorrhage may also occur after direct trauma to the eye, vigorous eye rubbing, improper use of contact lenses, or following ocular surgery such as refractive procedures (e.g., LASIK).
Systemic conditions such as hypertension, diabetes mellitus, and coagulation disorders, as well as the use of anticoagulant or antiplatelet medications like aspirin and warfarin, can increase the likelihood of developing a subconjunctival hemorrhage.
Recurrent episodes are more frequently seen in older adults or in individuals with fragile blood vessels, making this finding an important clinical clue when evaluating ocular health and the different causes of eye bleeding.
Management of subconjunctival hemorrhage
In most cases, a subconjunctival hemorrhage does not require specific medical treatment. The trapped blood is gradually reabsorbed by the body over a period of about one to three weeks, without leaving any impact on visual function.
Management focuses on identifying and addressing any underlying cause, such as controlling high blood pressure, reviewing the dosage of anticoagulant therapy, or avoiding excessive straining and untreated bouts of severe coughing.
Lubricating eye drops (artificial tears) can be used to relieve associated discomfort or dryness, although they do not significantly accelerate the resolution of the hemorrhage.
Patients are advised to avoid rubbing the eyes or wearing contact lenses during the episode, to protect the conjunctiva and reduce the risk of recurrence or secondary infection.
Urgent ophthalmologic evaluation is necessary if a subconjunctival hemorrhage is accompanied by severe eye pain, reduced vision, recurrent bleeding, significant eye trauma, or bleeding elsewhere in the body, as these may indicate a deeper ocular hemorrhage or an underlying systemic disorder requiring comprehensive assessment.
Anterior Chamber Hemorrhage (Hyphema)
Anterior chamber hemorrhage, known medically as hyphema, is the accumulation of blood in the narrow space between the cornea and the iris. It usually occurs after direct trauma to the eye, but may also develop following eye surgery or as a complication of chronic conditions such as hypertension and diabetes.
This type of ocular bleeding is considered one of the more serious forms of internal eye hemorrhage, as it can cause a sudden rise in intraocular pressure and threaten the health of both the cornea and the optic nerve if not treated promptly.
Patients typically notice a visible reddish layer or a clear fluid–blood level in front of the iris, often accompanied by blurred vision, eye pain, and marked sensitivity to light (photophobia).
Hyphema requires urgent evaluation by an ophthalmologist to assess the extent of bleeding, measure intraocular pressure, and initiate appropriate treatment. Management usually includes anti‑inflammatory eye drops, intraocular pressure–lowering medications, along with rest and avoiding bending over or strenuous physical activity.
Early detection and prompt treatment help reduce the risk of complications such as glaucoma and corneal damage, and significantly improve the chances of restoring normal vision.
What is hyphema?
Hyphema – also known as anterior chamber hemorrhage – is the accumulation of blood in the small space between the cornea and the iris, medically referred to as the anterior chamber of the eye.
This type of eye hemorrhage is particularly important because it is clearly visible as a layer or pool of blood in the front part of the eye, and may cause blurred vision or a temporary reduction in visual acuity.
Hyphema occurs when tiny blood vessels within or around the iris rupture and bleed, allowing blood to collect in the anterior chamber instead of mixing normally with the clear aqueous humor.
The hemorrhage may be mild and gradually resolve on its own, or it may be severe, filling a large portion of the anterior chamber and requiring urgent medical attention to prevent complications such as raised intraocular pressure or optic nerve damage.
Recognizing and understanding hyphema is a key component of evaluating intraocular hemorrhages, as it directly affects visual quality and the health of the anterior segment of the eye.
Causes of hyphema
Hyphema has multiple causes, but it is most commonly associated with direct trauma to the eye, such as a strong blow during sports, accidents, or work-related injuries, which can tear delicate blood vessels in the iris or ciliary body.
It is also a well‑known potential complication of eye surgery, such as cataract extraction or glaucoma surgery, where a mild anterior chamber bleed may occur postoperatively.
Certain systemic diseases, including hypertension, diabetes mellitus, and coagulation disorders, can make ocular blood vessels more prone to bleeding, thereby increasing the risk of hyphema as a form of intraocular hemorrhage.
Hyphema can also be secondary to primary eye diseases, such as intraocular tumors, iritis or uveitis, and retinal vascular disorders whose effects may extend to the anterior chamber.
In some uncommon cases, hyphema occurs spontaneously without an obvious trigger, particularly in individuals taking blood thinners or anticoagulant medications, underscoring the importance of regular ophthalmic follow‑up in this group.
Management of hyphema
Management strategies for hyphema depend on its severity and underlying cause, with the main goal being to protect the eye from complications such as elevated intraocular pressure or loss of vision.
In mild anterior chamber hemorrhages, the ophthalmologist may recommend conservative treatment: rest, sleeping with the head elevated, and using eye drops to reduce inflammation or dilate the pupil, while closely monitoring intraocular pressure.
If the hyphema is trauma‑related, medications that stabilize blood vessels or reduce inflammation may be prescribed, and the patient will be advised to avoid strenuous physical activity and bending over, as these can worsen bleeding within the anterior chamber.
In moderate to severe cases, or if the hemorrhage persists or intraocular pressure rises, a minor surgical procedure may be required to evacuate the blood from the anterior chamber, in order to protect the cornea and optic nerve and preserve vision.
Equally important is addressing the underlying cause of the hyphema, whether a systemic condition such as hypertension or diabetes, or a local ocular problem, since controlling these factors reduces the risk of recurrence and helps prevent other forms of intraocular hemorrhage and related complications.
Vitreous Hemorrhage
Vitreous hemorrhage is a type of intraocular bleeding that occurs when blood leaks into the clear, gel-like substance (the vitreous body) that fills the space between the lens and the retina. This can lead to blurred vision, the sudden appearance of dark floaters, or the sensation of a dark curtain obscuring part or all of the visual field.
This form of eye bleeding is most commonly associated with diabetic retinopathy, retinal tears or retinal detachment, and direct ocular trauma. It may also be linked, in some cases, to sudden spikes in blood pressure or blood-clotting disorders.
In mild cases, the body may gradually clear the hemorrhage on its own with rest and close ophthalmic follow‑up. However, dense or persistent vitreous hemorrhage may require surgical intervention, such as a vitrectomy, to remove the blood-filled vitreous, protect the retina, and reduce the risk of permanent vision loss.
Any sudden change in vision suggestive of vitreous hemorrhage warrants urgent assessment by an ophthalmologist, particularly in people with diabetes or a known history of retinal disease. Early diagnosis and prompt treatment are crucial to preserving vision and minimizing complications.

What is a vitreous hemorrhage?
A vitreous hemorrhage is bleeding into the clear, gel-like substance that fills the center of the eye, known as the vitreous body (or vitreous humor). It is one of the types of intraocular bleeding that can directly affect visual ability.
This bleeding occurs when tiny blood vessels in or around the retina rupture and leak blood into the vitreous. As a result, blood mixes with the vitreous gel and causes blurred vision, hazy eyesight, or the sudden appearance of dark or shadowy floaters within the visual field.
In mild cases, a vitreous hemorrhage may be limited in extent and gradually clear on its own over time. In more severe cases, however, it can lead to a sudden, partial, or even total loss of vision in the affected eye.
Vitreous hemorrhage can sometimes be an ocular emergency, because ongoing or recurrent bleeding may indicate a serious underlying problem in the retina or the intraocular blood vessels. This requires careful assessment by an ophthalmologist.
Understanding what vitreous hemorrhage is helps in recognizing it early and distinguishing it from other forms of ocular bleeding, thereby allowing the selection of the most appropriate treatment to preserve vision.
Causes of vitreous hemorrhage
The causes of vitreous hemorrhage are varied and depend on the patient’s age and general health, but the most common are related to retinal diseases and abnormalities of the intraocular blood vessels.
Diabetic retinopathy is one of the leading causes. Poorly controlled diabetes can lead to the growth of fragile, abnormal new blood vessels in the retina (proliferative diabetic retinopathy), which are prone to rupture and bleed into the vitreous cavity.
Another important cause is retinal tear or retinal detachment. When the retina tears or begins to detach, small retinal blood vessels may be disrupted, leading to sudden intraocular bleeding.
Vitreous hemorrhage may also result from direct ocular trauma, blunt injury to the head, retinal vein occlusion, or certain blood disorders and coagulopathies that affect normal blood clotting.
In some older adults, vitreous hemorrhage can occur without an obvious precipitating factor, especially in the presence of fragile retinal vessels or degenerative retinal changes.
Accurately identifying the cause of vitreous hemorrhage enables the ophthalmologist to design an appropriate management plan, helps prevent recurrence, and protects the eye from long‑term complications.
Treatment options for vitreous hemorrhage
Treatment of vitreous hemorrhage depends on the severity of the bleeding, its underlying cause, and the degree to which vision and daily visual function are affected.
In mild cases, the ophthalmologist may opt for close observation only, allowing time for the eye to gradually clear the blood on its own. Vision often improves over weeks to months, provided that strenuous physical exertion is avoided and any new visual changes are promptly reported.
If the hemorrhage is secondary to conditions such as diabetic retinopathy or a retinal tear, retinal laser treatment (photocoagulation) may be used to seal retinal breaks or treat abnormal neovascular vessels, thereby reducing the risk of ongoing or recurrent bleeding.
In more severe or persistent cases, where the accumulated blood significantly blocks light from reaching the retina, the ophthalmologist may recommend a vitrectomy. In this microsurgical procedure, the blood-filled vitreous gel is removed and replaced with a clear solution to restore a transparent visual pathway.
Managing the underlying cause is an essential part of therapy, including strict control of blood glucose in diabetes, treatment of hypertension, and regular follow‑up for chronic retinal diseases.
The choice of treatment is always based on a comprehensive eye examination, retinal imaging, and a careful evaluation of potential risks, with the main goal of preserving vision and preventing complications related to intraocular hemorrhage.
Retinal Hemorrhage
Retinal hemorrhage is bleeding within the light‑sensitive retinal layer at the back of the eye. It is considered one of the more serious types of ocular bleeding, as it can cause severe visual impairment or even permanent vision loss if not treated promptly.
Retinal hemorrhage most commonly occurs as a result of diabetic retinopathy, long‑standing hypertension, retinal vein or artery occlusion, or significant ocular trauma.
Symptoms may include the sudden appearance of floaters or dark spots in the visual field, acute blurring of vision, difficulty seeing fine details, and in some cases loss of part of the visual field.
Diagnosis is based on dilated fundus examination, along with retinal imaging such as fluorescein angiography and optical coherence tomography (OCT) to accurately localize the hemorrhage and assess its extent.
Treatment depends on the underlying cause and may include strict control of blood glucose and blood pressure, intravitreal injections of anti–vascular endothelial growth factor (anti‑VEGF) agents, retinal laser therapy, and in severe cases pars plana vitrectomy.
Early detection of retinal hemorrhage, together with regular follow‑up of patients with diabetes and hypertension, is crucial to preventing serious complications and preserving vision in the long term.
What is Retinal Hemorrhage?
Retinal hemorrhage is a type of intraocular bleeding that occurs when small blood vessels within the retina leak blood. The retina is the light-sensitive layer at the back of the eye responsible for capturing images and transmitting visual signals to the brain.
This condition is considered serious because it can directly impair visual acuity, leading to blurred vision, distorted images, or the appearance of floaters and dark spots in the field of vision.
Retinal hemorrhage can range from mild, with little to no noticeable symptoms, to severe, causing sudden or progressive loss of vision, depending on the location and extent of the bleeding.
Understanding retinal hemorrhage helps distinguish it from other types of ocular bleeding, such as vitreous hemorrhage or subconjunctival hemorrhage, which guides the choice of appropriate diagnostic and therapeutic approaches.
Recognizing retinal hemorrhage is particularly important in people with diabetes and uncontrolled hypertension, as they are at higher risk of damage to the small retinal vessels.
Causes of Retinal Hemorrhage
Retinal hemorrhage is most often associated with chronic systemic diseases that affect the ocular microvasculature, foremost among them diabetic retinopathy. Prolonged elevation of blood glucose levels leads to weakening, leakage, and rupture of the small retinal blood vessels.
Poorly controlled hypertension is another common cause. Persistent high blood pressure puts excessive strain on the vessel walls in the retina, increasing the likelihood of rupture and bleeding.
Other causes include retinal vein occlusion, hematological disorders such as coagulation abnormalities or severe anemia, as well as direct ocular trauma, contusions, or injuries related to accidents and high-impact sports.
In some cases, hemorrhage occurs due to the growth of fragile, abnormal new vessels (neovascularization), as seen in ischemic retinopathies, retinopathy of prematurity, or systemic diseases such as advanced kidney or heart disease.
Accurately identifying the underlying cause enables the ophthalmologist to develop a comprehensive management plan that goes beyond treating the hemorrhage itself to addressing the primary systemic condition driving the problem.
Management of Retinal Hemorrhage
Treatment strategies for retinal hemorrhage depend on the cause, location, and severity of the bleeding. Mild, limited hemorrhages may only require observation with regular eye examinations, alongside strict control of blood glucose, blood pressure, and other risk factors to prevent progression.
When retinal hemorrhage is associated with diabetic retinopathy or pathological neovascularization, retinal laser photocoagulation may be used to seal or ablate diseased blood vessels, reducing leakage of blood and fluid and helping stabilize or improve vision.
The ophthalmologist may also administer intravitreal injections of specific medications, such as anti–vascular endothelial growth factor (anti‑VEGF) agents, to inhibit abnormal vessel growth and treat associated macular edema. These therapies are widely used in retinal hemorrhage related to diabetes or retinal vein occlusion.
In advanced cases, or when there is significant vitreous hemorrhage obscuring vision, a pars plana vitrectomy may be indicated to remove the accumulated blood, restore a clear visual axis, and allow direct treatment of the retina.
Early diagnosis and regular follow‑up with a retina specialist are key to effective management of retinal hemorrhage and to preventing long‑term visual complications, as part of an integrated approach to ocular hemorrhages and preservation of sight.
Bleeding Behind the Eye
Bleeding behind the eye refers to hemorrhage occurring in the back part of the eyeball, particularly in the retina. It is often caused by high blood pressure, diabetes, or direct eye trauma, and is considered one of the more serious forms of ocular bleeding because it directly affects the retina and the optic nerve, which are essential for vision.
This type of bleeding may present as a sudden blurring of vision, the appearance of black floaters, or dark patches in the visual field. In some cases, however, the patient may not notice any symptoms in the early stages, which makes regular eye examinations crucial, especially for individuals with diabetes or hypertension.
Diagnosis of bleeding behind the eye relies on a detailed fundus examination, as well as imaging techniques such as optical coherence tomography (OCT) and fluorescein angiography. Early detection and management are vital to prevent serious complications, including partial or complete loss of vision.
Treatment of retinal hemorrhage or bleeding in the posterior segment of the eye may involve medications to control blood pressure or blood sugar levels, intravitreal injections, laser therapy, or surgical intervention in advanced cases. At the same time, it is essential to address the underlying cause of the bleeding to protect ocular health and preserve vision.
What is a hemorrhage behind the eye?
A hemorrhage behind the eye is a condition in which blood leaks into the deeper structures located behind the eyeball, such as the retina, vitreous body, or choroid, and can directly impair visual function.
This type of eye bleeding is usually not visible on simple inspection and is most often detected only through a specialized ophthalmic examination.
In this situation, blood accumulates in highly delicate areas responsible for capturing light and transmitting images to the brain, which may lead to blurred vision, the appearance of floaters or dark spots, or a sudden, partial, or complete loss of sight in the affected eye.
The severity of a hemorrhage behind the eye can range from a mild bleed that the body can gradually reabsorb on its own, to a severe hemorrhage requiring urgent medical intervention. Understanding this condition is therefore a key part of recognizing different forms of eye bleeding and how to deal with them at an early stage.
Causes of hemorrhage behind the eye
The causes of hemorrhage behind the eye are varied and include chronic systemic diseases, acute trauma, and factors involving the small blood vessels within the eye.
One of the most common causes is diabetic retinopathy, in which poorly controlled blood glucose levels weaken the retinal blood vessels, making them prone to leakage or rupture and resulting in bleeding behind the eye.
Long‑standing high blood pressure is also a major risk factor, as it increases the likelihood of rupture of the small vessels, leading to different types of intraocular hemorrhage, including retinal hemorrhage and vitreous hemorrhage.
Bleeding behind the eye may also occur after direct trauma to the eye or head, due to retinal vein occlusion, coagulation disorders, or the use of anticoagulant medications without proper medical supervision.
Some less common conditions, such as intraocular tumors or congenital vascular malformations, can also be among the causes of hemorrhage behind the eye, which underscores the importance of a thorough evaluation whenever there is any sudden change in vision.
Treatment options for hemorrhage behind the eye
Management of hemorrhage behind the eye depends on the underlying cause, the severity of the bleeding, and the exact location of the accumulated blood.
In mild cases, the ophthalmologist may opt for close observation while addressing the root causes—such as optimizing blood sugar and blood pressure control—since part of the hemorrhage can be gradually reabsorbed by the body over time.
In other situations, the physician may use intravitreal injections, such as anti‑VEGF (anti–vascular endothelial growth factor) agents, to help stop vascular leakage and reduce the risk of recurrent retinal bleeding.
Medical laser therapy (retinal photocoagulation) is used to treat certain types of intraocular hemorrhage, especially in the context of diabetic retinopathy or retinal vein occlusion, as it helps seal damaged vessels and protect the retina from permanent damage.
In cases of dense vitreous hemorrhage, a vitrectomy may be required to remove the accumulated blood and restore the passage of light to the retina. This is a surgical procedure performed by a retinal specialist.
Early initiation of treatment for hemorrhage behind the eye, combined with regular follow‑up with an ophthalmologist, significantly reduces the risk of permanent complications and helps preserve the best possible level of vision within a comprehensive approach to all types of eye bleeding.
When Is Eye Bleeding an Emergency?
Eye bleeding is considered an emergency when it appears suddenly and is accompanied by abrupt vision loss or marked visual blurring, or when you notice something like a dark curtain or moving shadow across your field of vision. This can indicate a vitreous hemorrhage or a retinal detachment.
It also becomes serious if the bleeding is associated with severe eye pain, intense headache, nausea or vomiting, or a sudden, pronounced redness of the eye. These signs may point to acute elevation of intraocular pressure or a significant internal eye injury.
Urgent medical attention or an immediate visit to the emergency department is essential if bleeding occurs after direct trauma to the eye or head, or if the person has diabetes, hypertension, or is taking blood thinners (anticoagulants), as these conditions increase the risk of retinal hemorrhage and its complications.
In all cases, any intraocular bleeding—whether in the conjunctiva, retina, or vitreous—accompanied by a noticeable change in vision requires prompt assessment by an ophthalmologist to identify the type of hemorrhage early and help prevent permanent vision loss.
Eye Hemorrhage Treatment at Batal Specialized Medical Complex
At Batal Specialized Medical Complex, eye hemorrhages are managed promptly and precisely to protect vision and minimize potential complications.
Treatment depends on the type and cause of the hemorrhage. The ophthalmologist begins with a comprehensive eye examination using advanced diagnostic tools such as fundus photography, ocular ultrasound, and optical coherence tomography (OCT).
In cases of simple subconjunctival hemorrhage, the physician usually opts for observation and lubricating eye drops, while addressing underlying risk factors such as uncontrolled hypertension or blood-thinning medications.
For vitreous hemorrhage or retinal bleeding caused by conditions like diabetic retinopathy or elevated intraocular pressure, treatment may include intravitreal injections of specialized medications, retinal laser photocoagulation, and, when necessary, pars plana vitrectomy to clear the blood and improve vision.
The complex also focuses on treating the underlying causes of eye bleeding, such as diabetic retinopathy, retinal vein or artery occlusions, and ocular trauma, supported by close follow‑up and an individualized treatment plan for each patient.
With a highly qualified team in ophthalmology and eye surgery, and state-of-the-art medical equipment, Batal Specialized Medical Complex provides comprehensive and safe care for all types of eye hemorrhages.



